
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
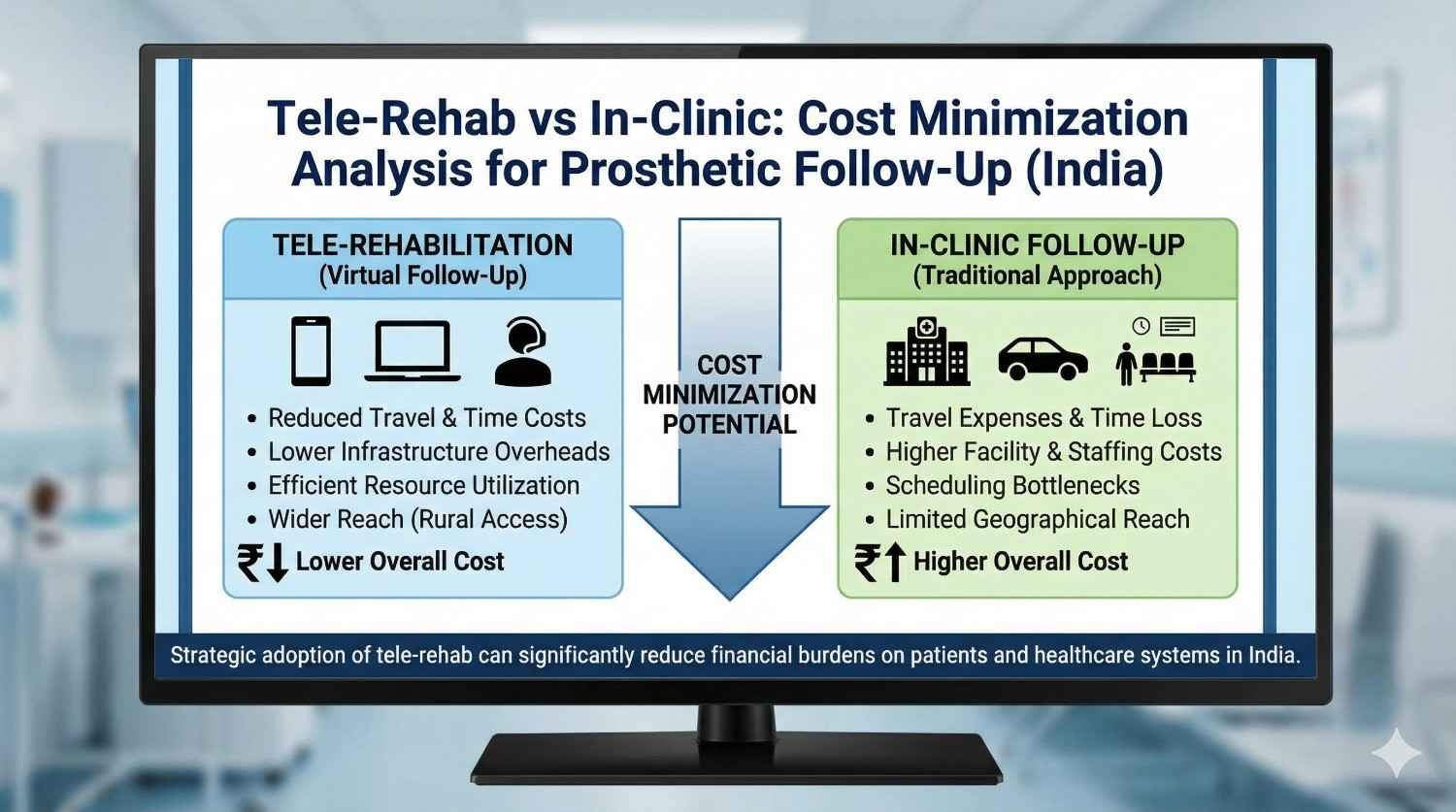
Follow-up care keeps a prosthetic user safe, confident, and independent. The question is simple: should that care happen online or in person? In India, where people often travel far for care, the way we choose matters. This article gives a clear, numbers-first way to decide. The tone is practical. The steps are easy to use. The goal is lower total cost without lowering outcomes.
India is big. Many users live hours away from the nearest clinic. Travel takes time, needs money, and breaks daily routines. Families juggle work, school, and caregiving. When a prosthetic user skips follow-ups, small problems become big. Sockets loosen. Skin breaks down. Batteries fail. Training slips. The user loses trust in the device. Then the device sits in a drawer. That is the most expensive outcome of all.
Tele-rehab can help. Video calls, photos, app-based tasks, and remote adjustments can solve most routine needs. But not all. Some issues need a socket check, a grip force test, or hands-on skin care. The right choice is not tele vs in-clinic. It is tele when safe, clinic when needed, and a smart mix for the rest.
Tele-rehab is planned care delivered over a phone or laptop. It includes video visits, guided home tasks, photo-based checks, and data review from the prosthesis or companion apps. In-clinic follow-up is a visit to a prosthetic center where a clinician examines fit, alignment, control signals, skin health, and device function, and gives training.
Both paths share the same goals: comfort, function, safety, and user joy. The difference is how we get there, how much it costs in money and time, and how often we need to repeat it.
Cost minimization analysis is simple. If two care paths achieve the same outcomes, choose the cheaper one. To do this well, we must count all costs, not only the clinic bill.
These include travel fares, fuel, tolls, parking, meals on the way, phone data, lost day wages, and a caregiver’s time. We should also count the cost of arranging a ride or missing a day of school. These are real costs even if no cash changes hands.
Clinics have room rent, power, staff time, and equipment upkeep. There is also the hidden cost of no-shows and late reschedules. Tele-rehab has platform fees, devices, data plans for staff, and training time to learn the workflow. Over time, tele can reduce idle time and smooth the schedule.
These include over-crowded outpatient departments, transport subsidies, and public health burdens from complications. Fewer infections, fewer pressure sores, and fewer device dropouts save money for the system.
To keep this practical, let us build a model you can copy into a spreadsheet. We will use round numbers in rupees. You can replace them with your own.
Let us define:
Now assign costs.
These are example numbers to illustrate the method. Change them to fit your reality.
These are not rules. They are levers. Adjust and see how your totals move.

Riya lives in Pune city, 12 km from a clinic. She uses a myoelectric hand. Her routine plan calls for six touchpoints in year one: one in person at one month, one in person at six months, four tele sessions in between.
Costs for two clinic visits:
Total for two clinic visits: 432 + 1,200 + 800 + 400 = 2,832.
Costs for four tele sessions:
Total for tele: 1,600 + 60 + 415 = 2,075.
Year total: 2,832 + 2,075 = 4,907.
What if all six were in clinic?
Total all-clinic: 9,792.
Savings with mixed plan: 9,792 − 4,907 = 4,885. This is more than the price of a good smartphone. The outcome is the same: a stable, confident user.
Arun lives 120 km away from the nearest center. He travels by bus with a family member.
Costs for one clinic visit:
Total per clinic visit: 3,000.
If he needs four touchpoints in six months, and two can be tele:
Total: 6,830.
All four in clinic would cost: 3,000 × 4 = 12,000.
Savings: 5,170. But the bigger win is time. Arun saves two full days away from work and home.
In real life, touchpoints are not fixed. Early months may need more. A new device, a new job task, or a growth spurt in teens can raise the count. A strong hybrid plan keeps the marginal cost of extra support low.
Assume an added two touchpoints due to a new job task. If both are tele:
The marginal cost difference is large. This is how tele protects both the family budget and adherence.
Many budgets forget small but real drains.
First, the cost of a missed appointment. The user may have already taken leave and paid for travel. A last-minute clinic emergency can push the slot. The same day, the user loses wages and morale. Tele slots are easier to shuffle on short notice. The friction cost is lower.
Second, caregiver burnout. Repeated school and work leave affects the family over time. Tele reduces the load, which improves long-term follow-up rates and device use.
Third, child care and elder care. When a parent travels to the clinic, someone else must cover care at home. That has a cost even if no cash is paid. Tele keeps care within reach.
Fourth, weather and safety. Heavy rain, heat waves, and late-night travel add risk. Tele avoids these risks for routine checks.
Fifth, the dropout effect. Every hurdle adds to the chance that a user says, “I will go next month,” and next month never comes. A small skin mark turns into a wound. A loose electrode becomes a control problem. Tele makes early help easy, so issues stay small.
Cost minimization only works if outcomes are equal. For many follow-ups, they are.
Tele matches clinic for:
Clinic is better for:
With clear triage rules, most users can shift at least half of their touchpoints to tele without losing quality.

You can use a simple yes/no flow in your front desk script.
Start with the user’s main concern. If there is pain, bleeding, swelling, heat, fever, or sudden loss of function, route to clinic. If the issue is training, signal control, minor redness, more battery drain, or routine check, route to tele. If unsure, offer a short tele screening first. If during screening any red flag appears, convert to an in-clinic slot.
This two-step method prevents unsafe delays and still saves the majority of travel.
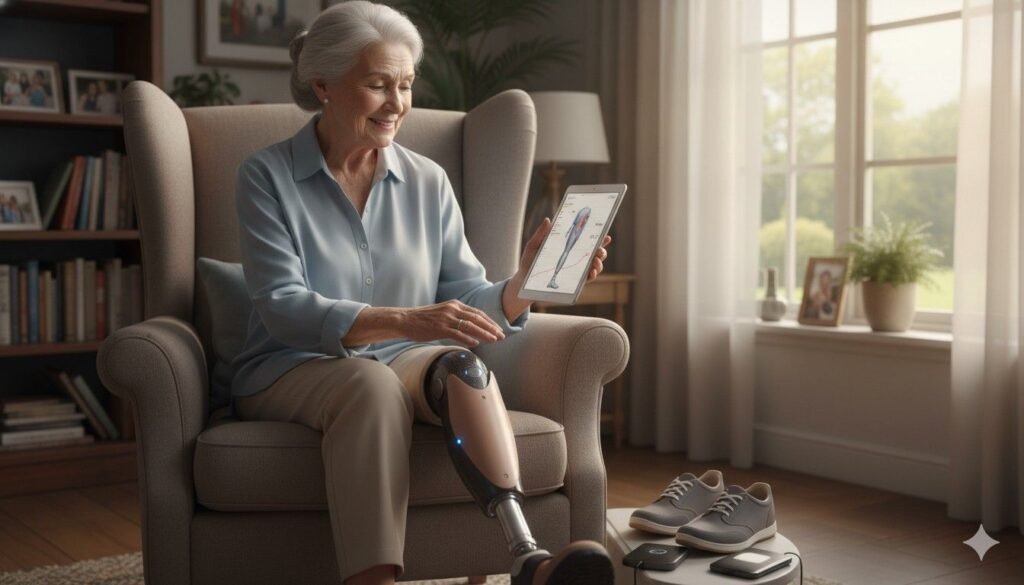
Tele does not need fancy gear. It needs simple, reliable tools that fit real life.
A mid-range Android phone, a stable 4G connection, and a quiet corner are enough for most sessions. Good lighting and a helper to hold the camera make skin photos clear. If the device can share data logs or simple status screens, the clinician can see patterns without extra hardware.
A good tele app is one that opens fast, uses little data, and does not crash on older phones. It should allow photo and short video uploads, a checklist of tasks, and secure chat. It should work in English and local languages. It should keep the user’s privacy safe.
Respect for data builds trust. Before the first tele visit, take clear consent. Explain what is collected, why it is collected, and how it is stored. Use secure channels for photos and reports. Avoid public messengers for private data. Give the user control to delete shared files when they want. Keep logs only as long as needed for care.
Trust also means showing up on time, speaking with warmth, and closing the loop. After each tele session, send a short summary and the next steps. This small step makes the user feel seen and cared for.
Some moments demand hands-on care. A new wound needs debridement advice and dressing. A cracked socket needs immediate inspection. A failing battery or a frayed cable needs a bench test and a safe swap. A large change in limb volume may call for a new liner or socket work. When safety is at stake, the clinic is the right place.
The role of tele here is to triage fast, book a priority slot, send travel prep tips, and reduce time at the clinic by completing paperwork and history online.
The smartest plan is simple. Start in clinic for fitting and early training. Move to tele for habit building and small tweaks. Come back to clinic for milestone checks and any red flag. Wrap the year with a full in-clinic service. This mix cuts travel while keeping touch high.
A common pattern that works well:
Adjust based on need. If the user starts a new job or a sport, add short tele sessions to fine-tune technique and settings. If skin is sensitive, add photo checks after long wear days. These extra tele touches are cheap and often prevent a costly clinic trip.
Our goal is simple: keep the user moving, smiling, and safe. We design our devices and workflows to make remote care easy.
For users of our Grippy bionic hand, we guide signal training in small, doable steps. We ask for short practice videos and give feedback the same day. Our Sense of Touch system helps users understand grip better, and we build those lessons into tele coaching so control becomes second nature at home and at work.
For those using our rehab tools like BrawnBand and our gamified rehab app, we set clear daily targets and track progress with light data. We flag when a user needs extra help and step in with a quick call. This reduces long gaps and keeps motivation high.
For centers we partner with, we share a ready-to-use tele workflow. It includes a triage checklist, template scripts for front desk, consent forms, photo guides, and follow-up summaries. It is designed for low bandwidth and busy days. We also train staff to read myoelectric patterns remotely and make safe decisions fast.
You can set up a cost-saving tele program in two weeks. Here is a simple path that works.
Start by mapping your most common follow-up visits. Mark which can be tele. Write your red flag list. Train your front desk to screen calls using two or three simple questions. Pick tele slots in the schedule and leave buffer time for overruns. Keep the first tele session to 20 minutes with a clear agenda. Use the last two minutes to state next steps and confirm the next check.
Build a photo guide for users. Show how to take a clear skin photo with a coin next to the area for size, under bright light, and at two angles. Ask for a 15-second video of control if needed. This improves accuracy and saves a lot of back-and-forth.
Set rules for converting tele to clinic. For example, if redness does not improve in 48 hours, book an in-clinic check. If a device fault persists after two tele tries, bring the user in for a bench test. Clear rules reduce decision fatigue and protect safety.
Track outcomes. Count issues resolved on tele, conversions to clinic, time to relief, and user satisfaction. Review every month. Small tweaks in your triage questions can boost success rates and shave costs further.
Tele should help your bottom line while improving care. Here is a quick way to see it.
Calculate your average cost per in-clinic follow-up slot, including staff time and room costs. Compare it to your tele slot cost. Add the savings from fewer no-shows because tele is easier to attend. Add the gain from filling last-minute gaps with tele users who can hop on a call. Clinics often find that a 40–60% tele mix increases total completed follow-ups per week without adding staff. Better follow-up leads to happier users, more referrals, and fewer urgent fixes that disrupt the day.

If you support prosthetic users at scale, a tele-first model reduces dropouts and complication claims. You can sponsor data packs, lend simple tripods for phones, and fund a tele coordinator at partner clinics. Tie payments to completed touchpoints and stable outcomes, not only device delivery. This aligns incentives and lowers true cost of care over the year.
Pick a bright spot with a plain background. Clean the camera lens. Keep the charger handy. Have a helper if possible. Wear a short-sleeved top so the limb is easy to see. Note down any questions beforehand. If the skin is red, wash your hands, take a clear photo with a coin for scale, and share it in the app. Keep your calendar open for a follow-up call if needed. These small steps make the call smooth and the advice accurate.
Tele is perfect for habit building. Set tiny goals: two short practice blocks each day, one in the morning and one in the evening. Use real-life objects from your daily routine: a steel glass, a key, a pen, a wallet, a spoon. Celebrate small wins. If a move is hard, send a 15-second video. We will mark the exact point to relax or to switch grip. This makes learning fast and fun.
When a device needs service, tele helps you act early. Many issues start small: a loose cable, a weak signal, a liner that has stretched. A quick video and a guided check can fix these at home or catch them before they turn into a full breakdown. If a part swap is needed, we plan the clinic visit so parts and tools are ready. You spend less time waiting and more time living.
Tele-rehab is not a shortcut. It is a smart way to deliver the same outcomes with less strain on time, money, and energy. In India, where travel is long and days are full, a tele-first, clinic-when-needed plan lowers total cost without lowering care. When we count every rupee and every hour—fares, lost wages, caregiver time, no-shows, weather delays—the hybrid model wins again and again.
Here is the clear takeaway: start in clinic for fitting and safety, shift routine coaching and minor checks to tele, and return in person for milestones and red flags. This simple pattern keeps skin safe, signals stable, and confidence high. It also protects family budgets and clinic capacity. The numbers are on your side, and the experience feels easier for everyone.
For users and families, tele makes follow-up doable. You get quick answers, timely tweaks, and fewer missed days at work or school. For clinics, a planned tele mix cuts idle time, reduces last-minute gaps, and improves completion rates. For payers and CSR teams, the model reduces dropouts and complications while funding only what truly helps—completed touchpoints and stable outcomes.
What matters most is discipline: clear triage rules, short and focused sessions, strong consent and privacy, simple photo guides, and fast escalation when needed. Do this well and you will see fewer wounds, fewer breakdowns, and more daily use of the prosthesis. That is real value—human and financial.
At RoboBionics, this is how we work. Our devices and workflows are built for remote coaching, quick feedback, and low bandwidth realities. We will help you set up a safe triage tree, train your team, and measure results month by month. For users, we keep practice simple and personal so progress sticks at home and on the job.
If you are ready to act, choose one next step today. Clinics can map follow-ups and launch a pilot tele block next week. Payers can sponsor data packs and a tele coordinator. Families can book a tele screening to plan their year of care and costs. Small moves now prevent big bills later.
Care should feel close, kind, and practical. A hybrid pathway makes it so. Let us help you design it, measure it, and keep it working—quietly, reliably, and affordably.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.