
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
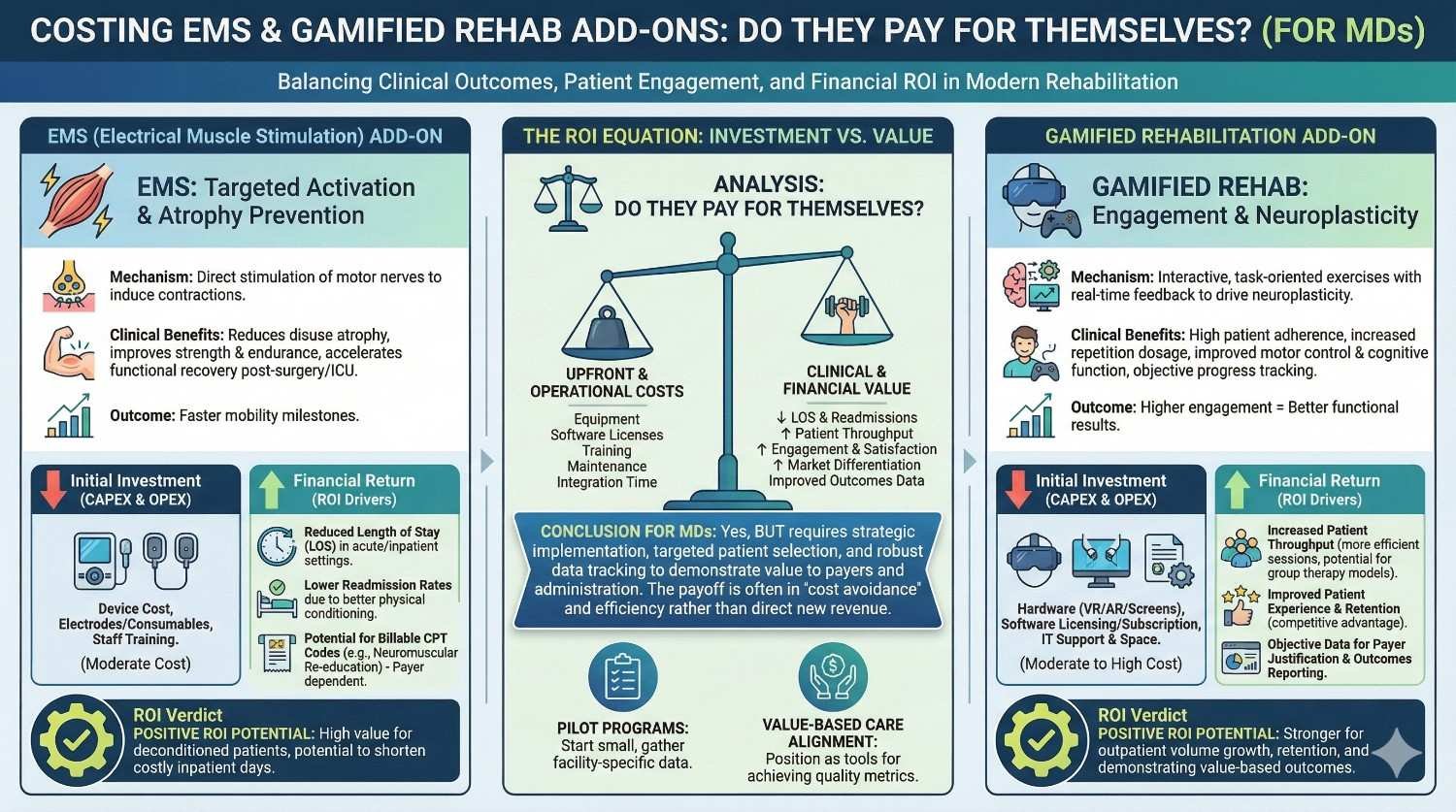
When a prosthesis is prescribed, the real work starts after delivery. Muscles must relearn, confidence must return, and habits must form. This is where EMS devices and gamified rehab tools enter the conversation. Many doctors ask a fair question: do these add-ons actually pay for themselves, or do they only add cost? This article answers that question in plain terms. It breaks down costs, time, outcomes, and real-world use so MDs can decide when EMS and gamified rehab make clinical and financial sense.

A prosthesis has value only when it becomes part of daily life.
If the patient avoids wearing it, even the best device fails in real terms.
Poor rehab is one of the main reasons for non-use.
Weak muscles, low control, and fear of failure slowly push the device aside.
When rehab improves, usage improves.
Usage is where value is created.
The first few weeks after fitting shape everything that follows.
Patients either build confidence or develop avoidance.
Strong early rehab shortens the learning curve.
It reduces frustration and emotional fatigue.
EMS and gamified rehab target this early window.
That timing is critical for outcomes.
When rehab fails, costs rise quietly.
Extra visits, repeated adjustments, and longer therapy cycles add up.
When rehab works, follow-ups reduce.
Patients progress faster with fewer complications.
This is where add-ons must be judged.
Not by price, but by downstream impact.
Electronic Muscle Stimulation helps activate weak or unused muscles.
It sends controlled signals that cause muscles to contract.
For amputees, this helps reawaken muscle memory.
It prepares muscles for myoelectric control and endurance.
EMS does not replace exercise.
It supports and accelerates it.
EMS is most useful in early and mid rehab.
Especially when muscle activation is poor or delayed.
It helps patients who struggle with voluntary contraction.
It also supports symmetry and control.
Doctors often use EMS to bridge gaps.
It fills the space between intent and action.
EMS is not magic.
It does not work without guidance and consistency.
Poor placement or irregular use reduces benefit.
Patient education matters.
Understanding these limits prevents overpromise.
It keeps expectations realistic.
Rehab fails as often due to boredom as due to pain.
Repetition without engagement drains motivation.
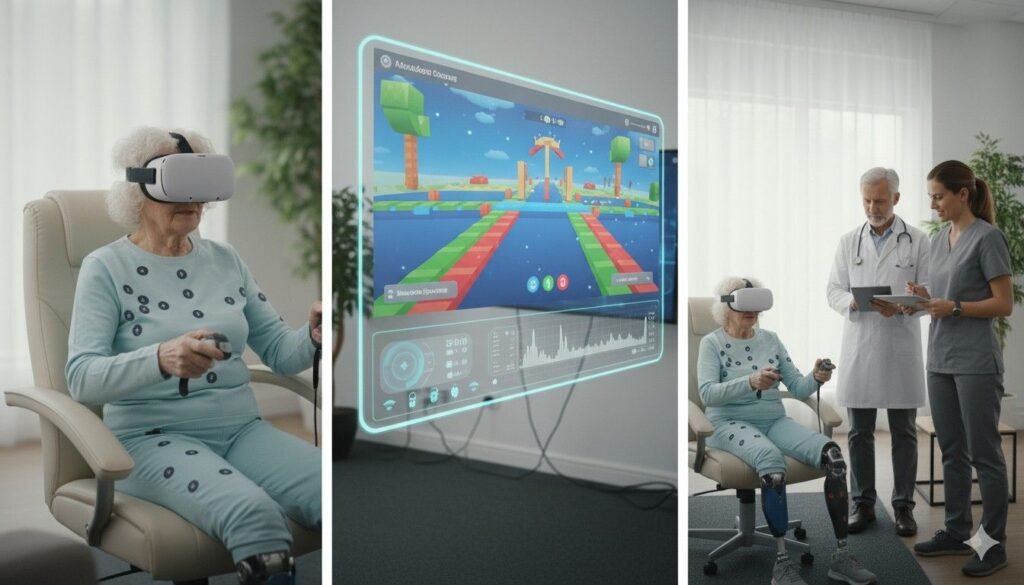
Gamified rehab turns exercises into simple challenges.
Points, progress, and feedback keep patients involved.
This motivation is not childish.
It is practical and effective.
When rehab feels rewarding, patients do more of it.
Higher frequency leads to faster gains.
Gamified tools also provide structure.
They reduce dependence on constant therapist supervision.
For home-based rehab, this matters a lot.
Consistency improves outcomes.
Gamification is not a substitute for assessment.
It cannot correct poor technique alone.
Doctors and therapists must still guide.
Tools support care, they do not replace it.
Used well, they amplify effort.
Used poorly, they become distractions.
EMS devices have an upfront cost.
This may be borne by the clinic or patient.
Some clinics bundle EMS into rehab packages.
Others prescribe them as add-ons.
The key question is not the price alone.
It is what the cost replaces.
Gamified rehab often involves an app or system.
Costs may be per patient, per month, or per license.
At first glance, this looks like extra spend.
But it often replaces therapist time.
Doctors should compare like with like.
Time is also a cost.
Missed appointments, dropouts, and slow progress all cost money.
They rarely appear on invoices.
EMS and gamified rehab reduce these hidden losses.
This is where payback often happens.
Ignoring hidden costs leads to wrong conclusions.
They must be counted.

Patients who activate muscles earlier need fewer sessions.
Therapists spend less time on basic activation.
This frees time for higher-value training.
Clinics become more efficient.
For doctors, this means smoother progress.
For patients, faster confidence.
Time saved is real value.
It has cost implications.
For myoelectric prostheses, signal quality matters.
Weak signals delay control mastery.
EMS improves signal readiness.
This reduces frustration and device rejection.
Lower rejection rates protect prosthetic value.
This alone can justify EMS cost.
Device abandonment is the most expensive outcome.
EMS helps prevent it.
Weak muscles contribute to poor posture and overuse injuries.
These lead to pain and extra visits.
EMS-supported rehab improves balance.
This reduces secondary complaints.
Fewer complaints mean fewer interventions.
Costs drop quietly.
Most rehab happens at home, not in clinics.
Without structure, compliance drops.
Gamified rehab provides daily prompts and feedback.
Patients stick with routines longer.
Higher compliance means faster gains.
This shortens total rehab duration.
Shorter rehab reduces overall cost.
Value emerges gradually.
Therapists do not need to chase patients constantly.
Progress can be tracked remotely.
This allows therapists to focus where needed most.
Care becomes more targeted.
For clinics, this improves capacity.
More patients can be supported without burnout.
Efficiency improves without lowering care quality.
That is meaningful ROI.
Patients who enjoy rehab often continue longer.
Strength and control improve beyond minimum levels.
These gains protect prosthetic use over years.
Longevity improves.
Long-term function reduces replacement pressure.
That has large cost implications.
Doctors worry about affordability.
This concern is valid.
However, small upfront costs can prevent large future costs.
The comparison must be explained clearly.
Patients accept add-ons when benefits are clear.
Transparency matters.
Framing is important.
Honesty builds trust.
Some doctors worry patients will not use these tools.
This happens when tools are poorly introduced.
Proper onboarding improves usage.
So does follow-up.
Gamified rehab actually improves compliance for many.
It reduces this risk, not increases it.
Selection matters.
Not every patient needs every tool.
MDs already manage many variables.
Adding tools can feel overwhelming.
The key is integration, not addition.
EMS and gamified rehab should fit existing workflows.
Simple protocols work best.
Complexity reduces adoption.
If a patient already has strong control and habits,
additional tools may add little value.
In such cases, basic exercises may suffice.
Add-ons may not justify cost.
Doctors should be selective.
Not every case needs technology.
Judgment matters.
Overuse reduces credibility.
Some patients resist all rehab.
No tool can fix this fully.
If engagement is absent, ROI drops.
Tools cannot replace motivation entirely.
Doctors should assess readiness.
Tools should support willing users.
Screening improves outcomes.
It avoids waste.
Tools without guidance fail.
Poor instruction leads to misuse.
If clinics cannot support usage,
benefits fall.
Implementation matters as much as selection.
Support determines success.
Consider a below-elbow amputee starting with a myoelectric hand who shows weak and inconsistent muscle signals in the first two weeks. Without additional support, this patient typically needs more in-clinic sessions, repeated recalibration, and longer supervised training before basic control feels natural. Each extra visit adds cost, time off work, and frustration, which quietly increases the risk of device rejection.
When EMS is introduced early, muscle activation improves faster and signal quality stabilizes sooner. The patient reaches functional control in fewer sessions, and home practice becomes more productive. Even if the EMS device adds an upfront cost, the reduction in extra therapy visits and the lower risk of abandonment often outweigh that cost within the first few months. For the MD, the clinical trajectory becomes smoother and more predictable, which itself has value.
A younger patient may have good physical potential but poor follow-through with exercises at home. Traditional paper-based rehab plans often fail here, leading to slow gains and repeated counseling visits that drain both patient and clinic energy. Over time, the total rehab duration stretches, increasing indirect costs that are rarely counted.
Introducing gamified rehab in such cases changes behavior more than physiology. The patient practices more often because the activity feels structured and rewarding, not because they are reminded again and again. Over weeks, strength and coordination improve faster, and therapist time shifts from motivation to refinement. In this scenario, the gamified platform pays for itself by shortening rehab timelines and reducing dropouts, even though the tool itself may appear optional at first glance.
Patients who live far from the clinic face a different cost structure. Missed visits, delayed corrections, and long gaps in therapy are common, and these gaps often lead to suboptimal outcomes that later require intensive correction. The financial and emotional cost of travel compounds the problem.
For such patients, a combination of EMS and gamified rehab can act as a force multiplier. EMS supports muscle work without constant supervision, while gamified rehab provides daily structure and remote visibility. The clinic intervenes only when needed, rather than routinely. In these cases, the add-ons reduce travel-related costs and prevent deterioration between visits, which makes their value clear even if direct billing does not capture it fully.
Instead of starting with the price of EMS or a rehab app, MDs should start by asking what usually goes wrong in similar patients. Is it slow muscle activation, poor home compliance, repeated visits, or device non-use? Each of these problems already has a cost, even if it is not formally billed.
Once the common failure point is identified, the add-on can be evaluated as a preventive tool rather than an extra expense. If EMS reduces three additional therapy sessions, or if gamified rehab prevents one major dropout, the comparison becomes clearer and more honest. This reframing makes ROI visible where it was previously hidden.
Many rehab-related costs emerge over time, not at once. A patient who progresses slowly may cost the same per visit but far more over six months than one who progresses steadily. EMS and gamified rehab often compress timelines rather than eliminate steps.
MDs should compare total duration of rehab with and without add-ons, rather than comparing per-session costs. When timelines shorten, indirect savings appear in fewer adjustments, fewer complaints, and better long-term use. This time-based comparison is often where add-ons justify themselves most clearly.
The most expensive outcome in prosthetics is not an extra rehab session, but a device that is rarely used or fully abandoned. Any intervention that meaningfully reduces this risk has outsized value, even if its upfront cost seems modest.
EMS and gamified rehab both improve early confidence and control, which are strong predictors of long-term use. When MDs include prosthetic survival and sustained use in their mental ROI calculation, the balance often shifts in favor of these tools, especially for higher-end devices.

Patients are sensitive to feeling upsold, especially in prosthetic care where costs are already high. EMS and gamified rehab should never be positioned as premium extras or optional luxuries. Instead, they should be framed as support tools that make the main treatment work better.
When MDs explain that these tools are meant to reduce struggle, shorten rehab, or avoid repeat visits, patients understand the intent. This framing keeps the conversation clinical and ethical, rather than commercial. Clarity of purpose builds acceptance.
Not every patient will benefit equally from every add-on, and MDs should say this openly. Explaining who benefits most, and why, helps patients make informed decisions without pressure. It also protects the clinician’s credibility.
When patients hear both the potential benefit and the limits, trust increases. Those who choose the add-on are more likely to use it properly, which in turn improves outcomes and ROI. Transparency is not a barrier to adoption; it is a prerequisite for it.
The fastest way to undermine the value of EMS or gamified rehab is to prescribe them to everyone without discrimination. This leads to misuse, disappointment, and skepticism among patients and staff.
MDs should develop simple internal criteria for when these tools are most useful, such as early myoelectric users, low-adherence patients, or those with limited access to frequent therapy. Selective use preserves value and keeps outcomes strong. Judgment is what turns tools into treatment.
EMS and gamified rehab work best when they are embedded into existing rehab plans, not layered on top as separate programs. Simple protocols that define when to start, how often to use, and when to reassess reduce confusion for both patients and staff.
Consistency matters more than sophistication. When everyone follows the same basic approach, outcomes become predictable and easier to evaluate. Complexity, on the other hand, increases drop-off and weakens ROI.
Therapists are the bridge between prescription and daily use. If they are confident and comfortable with EMS and gamified rehab tools, patients follow. If therapists are unsure, tools remain underused.
Short, focused training sessions and clear escalation paths help therapists integrate these tools naturally. When therapists see faster progress and fewer repetitive sessions, they become advocates rather than skeptics. This cultural shift is essential for payback.
Clinics do not need heavy analytics to know whether these add-ons are working. Simple checks on progress, usage, and patient confidence are enough to guide decisions. Regular but light monitoring allows early correction without creating administrative burden.
Over time, clinics develop an intuitive sense of which patients benefit most. This feedback loop strengthens prescribing judgment and improves cost-effectiveness organically.
The real cost of rehabilitation decisions rarely shows up in the first month. It appears over years, through how well the patient continues to use the prosthesis, how often repairs are needed, and how confident the patient feels in daily life. Early rehab quality strongly shapes these long-term patterns. When muscles are well conditioned and control is learned correctly, users rely on their prosthesis naturally instead of avoiding it during stress or fatigue.
EMS and gamified rehab influence this early phase in a quiet but lasting way. They improve control consistency and confidence, which reduces compensatory movements and overuse of the sound limb. Over years, this lowers secondary problems like shoulder pain, back strain, and posture issues. These problems are expensive to treat and emotionally draining for patients. From a long-term economic view, preventing even a fraction of these issues changes the total cost picture significantly.
A prosthesis that is used correctly and confidently tends to last longer in functional terms. Users who struggle with control often subject devices to abnormal loads, sudden movements, and misuse, which increases wear and breakdown. Over time, this leads to earlier replacement or major repairs.
By improving early muscle control and coordination, EMS and gamified rehab indirectly protect the device itself. Fewer breakdowns mean fewer emergency visits and lower service burden. For higher-cost devices, this effect alone can justify the initial rehab add-on cost. MDs who think in terms of device lifespan, not just rehab completion, often see the value more clearly.
One of the least discussed but most important economic outcomes is patient independence. A patient who regains function faster and with confidence returns to work sooner, participates more fully in family life, and depends less on caregivers. These gains rarely appear in clinic accounts, but they matter deeply to patients and society.
EMS and gamified rehab often accelerate this return to independence by making early progress visible and motivating. When patients see themselves improving week by week, they invest more effort. Over years, this translates into better functional ceilings, not just quicker starts. For MDs, this is where clinical impact and economic sense meet.
Most payers do not openly advertise support for rehab add-ons, but they strongly dislike failure outcomes such as device abandonment, repeated claims, and frequent follow-ups. These failures increase costs and administrative load.
When EMS and gamified rehab reduce these failure modes, they align quietly with payer interests. Even if the add-on itself is not reimbursed directly, its effect on reducing downstream claims is valued. MDs who understand this dynamic can frame rehab add-ons as risk-reduction tools rather than cost increases when speaking with payers or hospital administrators.
Public schemes focus heavily on upfront cost control, but they also face pressure to show real-world benefit. Devices that are issued but not used undermine the credibility of these programs. While schemes may not explicitly fund EMS or gamified rehab today, outcomes data increasingly matter.
MDs who document improved adherence, reduced follow-ups, and better function build a case for future inclusion of structured rehab support. From a systems perspective, add-ons that improve outcomes strengthen the overall value of prosthetic programs. This long view is important when advocating for patients within constrained schemes.
Private insurers are slowly moving toward bundled and episode-based thinking, where the total cost of care matters more than individual line items. In such models, tools that reduce overall rehab duration and complications are attractive.
EMS and gamified rehab fit well into this logic when positioned correctly. Instead of being billed as extras, they are seen as enablers of efficient care. MDs who speak this language help clinics and patients navigate coverage discussions more effectively.

Before considering any add-on, MDs should ask what is most likely to limit success for this patient. Is it weak muscle activation, poor motivation, limited access to therapy, or early frustration with control? Each risk points to a different solution.
EMS is most useful when physiology is the bottleneck. Gamified rehab is most useful when behavior and adherence are the bottleneck. When both risks are present, combining them often makes sense. This risk-first thinking keeps decisions clinical and focused.
MDs should mentally estimate what failure looks like for this patient. Extra visits, delayed independence, device rejection, or chronic pain all have costs. These costs may be paid by the clinic, the patient, or the system, but they are real.
Once the cost of failure is visible, the cost of prevention becomes easier to justify. EMS and gamified rehab should be seen as insurance against predictable problems, not as optional enhancements. This shift in thinking clarifies many decisions.
Rehab add-ons should never be prescribed and forgotten. Early reassessment is key. If a patient is progressing faster than expected, the add-on can be tapered. If progress is still slow, support can be intensified.
This adaptive approach protects value. It ensures tools are used only as long as they are needed, which improves both outcomes and cost control. MDs remain in charge, not the tools.
EMS and gamified rehab are not about technology for its own sake. They are about reducing friction in one of the hardest parts of prosthetic care: turning a device into a habit. When used thoughtfully, they shorten learning curves, protect expensive prostheses, and reduce the emotional and financial cost of slow or failed rehab.
They do not pay for themselves in every case, and they should not be prescribed automatically. But in the right patients, at the right time, they often return more value than they cost, especially when long-term outcomes are considered. The key is judgment, not enthusiasm.
At RoboBionics, we see these tools as part of a broader rehab ecosystem, not as add-ons pushed for revenue. Our focus is on helping MDs choose interventions that genuinely improve outcomes and respect patient resources. When rehab works well, everything else in prosthetic care becomes easier, calmer, and more sustainable.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.