
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
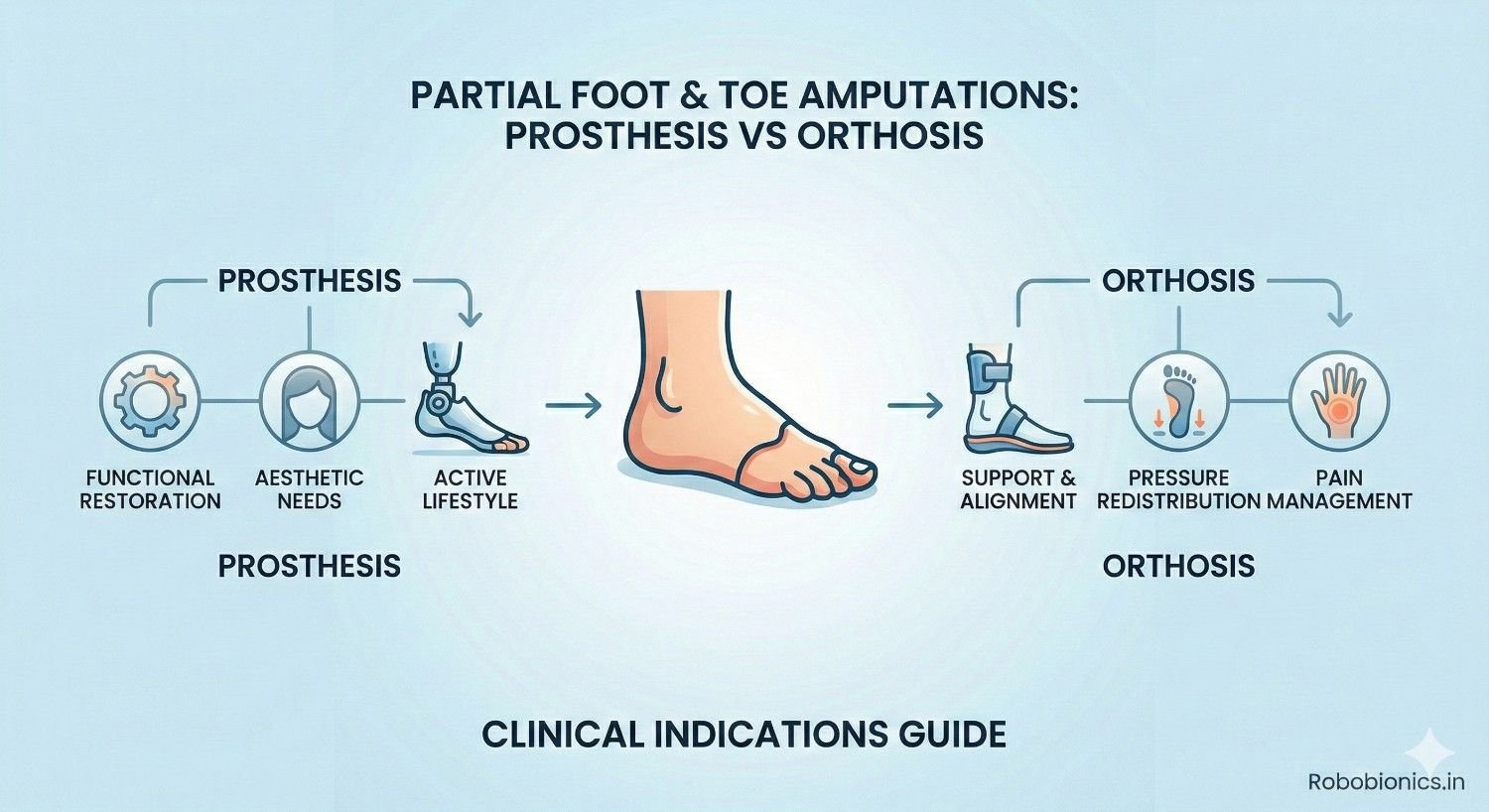
Partial foot and toe amputations are often seen as minor compared to higher-level limb loss, but their impact on walking, balance, and long-term foot health can be significant. Losing even a small part of the foot changes how weight is transferred, how muscles work, and how stable each step feels. This is why deciding between a prosthesis and an orthosis after partial foot or toe amputation is never a simple choice.
At Robobionics, we frequently meet patients who are told they may not need any device at all, only to develop pain, skin breakdown, or walking problems months later. We also see patients placed into prostheses that are heavier or more complex than needed, which reduces comfort and daily use. The real challenge lies in understanding when a prosthesis is truly required and when a well-designed orthosis can offer better function and protection.
This article focuses on partial foot and toe amputations and explains the clinical indications for choosing a prosthesis versus an orthosis. It looks closely at how different amputation levels affect gait, how load is redistributed across the foot, and how device choice influences long-term outcomes. The goal is clarity, not complexity.
If you are a doctor, therapist, or patient navigating this decision, this guide will help you understand the functional differences and make choices that support comfort, safety, and durability. The right solution is not about replacing what is lost, but about restoring stable and confident movement.
Even a small loss in the foot changes how the body moves.
The toes and forefoot play a major role in balance, push-off, and shock absorption during walking.
When part of the foot is missing, the body must quickly adapt to a new load pattern.
Patients often feel unstable without clearly understanding why.
This instability may not appear immediately but develops over weeks or months.
Early understanding helps prevent long-term problems.
Most partial foot and toe amputations happen due to diabetes, infection, or poor blood flow.
Trauma and tumors are less common but still important causes.
The underlying cause strongly affects healing and device choice.
Patients with diabetes often have nerve loss and poor circulation.
This increases the risk of skin breakdown after amputation.
Device decisions must protect the remaining foot carefully.
Leaving a partial foot amputation unsupported can cause secondary damage.
Excess pressure shifts to areas not designed to carry it.
This leads to ulcers, joint pain, and altered walking patterns.
Early intervention with the right device prevents these issues.
Waiting until pain develops often makes correction harder.
Proactive planning protects long-term mobility.
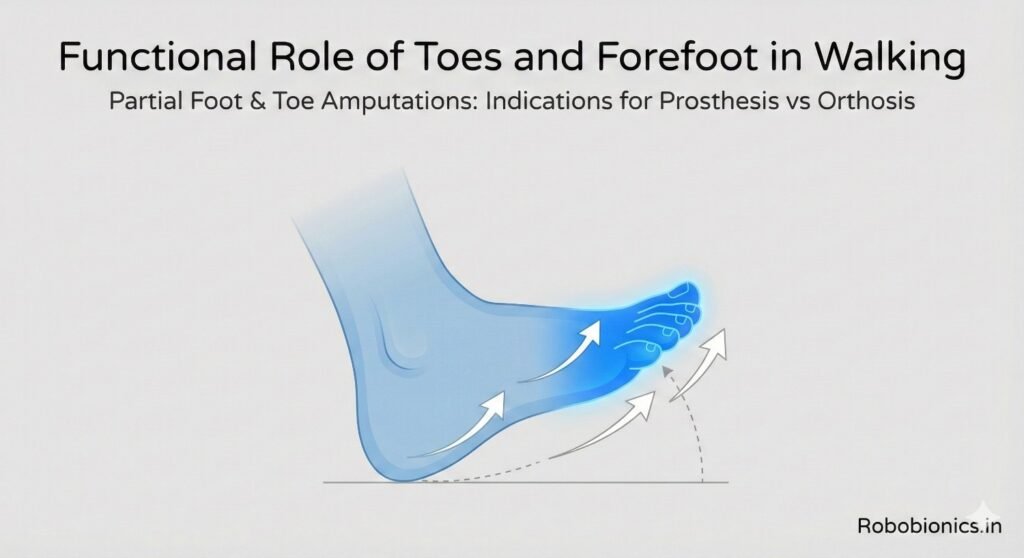
Toes help stabilize the body during standing and slow walking.
They widen the base of support and provide sensory feedback.
Loss of toes reduces this natural balance system.
Patients may feel fine on flat ground but struggle on uneven surfaces.
Turning and stopping become less controlled.
These issues increase fall risk over time.
The forefoot is critical during the push-off phase of walking.
It stores and releases energy with each step.
Loss of forefoot length reduces walking efficiency.
Patients often compensate by overusing the ankle or knee.
This increases fatigue and joint strain.
Over time, pain may develop in other areas.
Partial foot loss often leads to uneven walking patterns.
Stride length and timing change unconsciously.
The body favors the intact side.
Gait asymmetry increases stress on hips and lower back.
These changes may not cause pain immediately.
Long-term effects can be significant.
Single or multiple toe amputations seem minor but still affect balance.
Loss of the big toe has the greatest impact.
It alters push-off and stability significantly.
Smaller toe losses may cause subtle changes.
These changes accumulate over time.
Proper support helps reduce compensation.
Toe amputations often do well with orthotic solutions.
Prostheses are rarely required at this level.
However, assessment must be individualized.
Ray amputations remove a toe and part of the metatarsal.
This shortens the forefoot and shifts weight laterally or medially.
Balance becomes more difficult.
Patients often develop calluses or ulcers at new pressure points.
Footwear alone is usually insufficient.
Support must control load distribution.
At this level, advanced orthoses or prosthetic fillers may be needed.
The decision depends on stability and skin tolerance.
Functional testing guides choice.
Transmetatarsal amputations remove a large part of the forefoot.
Push-off is severely reduced.
Walking becomes less efficient.
Midfoot amputations further shorten lever arm length.
The ankle must work harder to compensate.
Energy cost rises noticeably.
These levels often require prosthetic solutions.
Orthoses alone may not provide enough leverage.
Stability and protection become priorities.
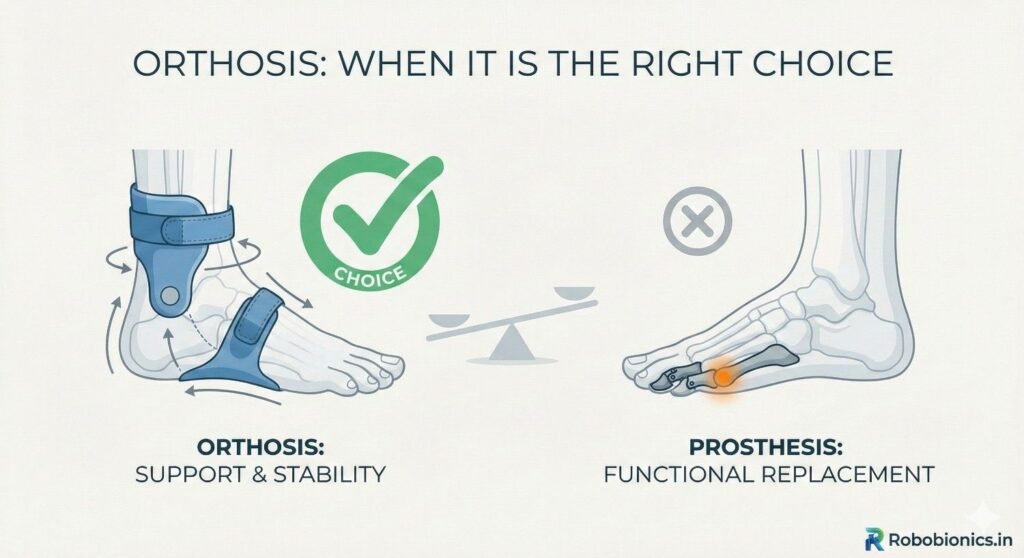
An orthosis supports and protects the remaining foot.
It redistributes pressure and improves alignment.
It works within the shoe.
Orthoses preserve natural foot movement as much as possible.
They are lighter and easier to manage.
This makes them attractive for early intervention.
Orthoses aim to prevent further damage.
They are protective rather than replacing missing anatomy.
Their role is often underestimated.
Orthoses work well when enough foot length remains.
Patients must have reasonable balance and strength.
Skin condition must tolerate shoe-based support.
Toe and partial ray amputations often respond well.
Early forefoot loss may still benefit from orthoses.
Comfort and stability guide this choice.
Patients with good ankle control usually do better.
Orthoses rely on existing joints.
Functional testing confirms suitability.
Orthoses are easier to wear and maintain.
They fit into standard footwear.
This improves daily compliance.
They allow more natural walking patterns.
Patients often feel less restricted.
Adaptation is quicker.
Orthoses also allow easy adjustments.
Changes in foot shape can be accommodated.
This flexibility is valuable in diabetic patients.
Orthoses cannot replace lost push-off power.
When forefoot length is too short, leverage is insufficient.
Walking remains inefficient.
Patients may still feel unstable despite good orthotic design.
Fatigue appears quickly.
Compensation increases.
At this point, orthoses may delay necessary prosthetic intervention.
Recognizing failure early is important.
Escalation improves outcomes.
Poorly designed orthoses can create pressure points.
This is dangerous in patients with reduced sensation.
Ulcers may develop unnoticed.
Frequent review is essential.
Skin must be monitored closely.
Early signs require immediate adjustment.
Orthoses are only safe when properly fitted.
Generic solutions often fail.
Customization is critical.
As amputation level moves proximally, orthoses lose effectiveness.
They cannot restore lever length.
They only cushion what remains.
At transmetatarsal and midfoot levels, this becomes clear.
Patients struggle with stairs and uneven ground.
Prosthetic solutions often work better.
Doctors must recognize this threshold.
Delaying prosthetic fitting increases strain.
Timely transition improves function.
A partial foot prosthesis replaces lost length and shape.
It restores a lever for push-off.
This improves walking efficiency.
The prosthesis works as an extension of the foot.
It often includes a filler and support shell.
This stabilizes the ankle and foot.
Prostheses shift load away from vulnerable areas.
They protect the remaining foot.
This is crucial in high-risk patients.
Prostheses are indicated when forefoot loss is significant.
Instability during walking is a key sign.
Failure of orthotic management also guides this decision.
Patients with transmetatarsal or midfoot amputations often need prostheses.
Energy loss becomes too great otherwise.
Balance improves with added structure.
Skin health also influences the choice.
Prostheses can offload pressure effectively.
This reduces ulcer risk.
Prosthetic users often walk more symmetrically.
Stride length improves.
Fatigue decreases.
Stability increases during standing and turning.
Confidence improves noticeably.
This encourages activity.
Prostheses also support long-term joint health.
They reduce compensatory stress.
This protects knees, hips, and back.
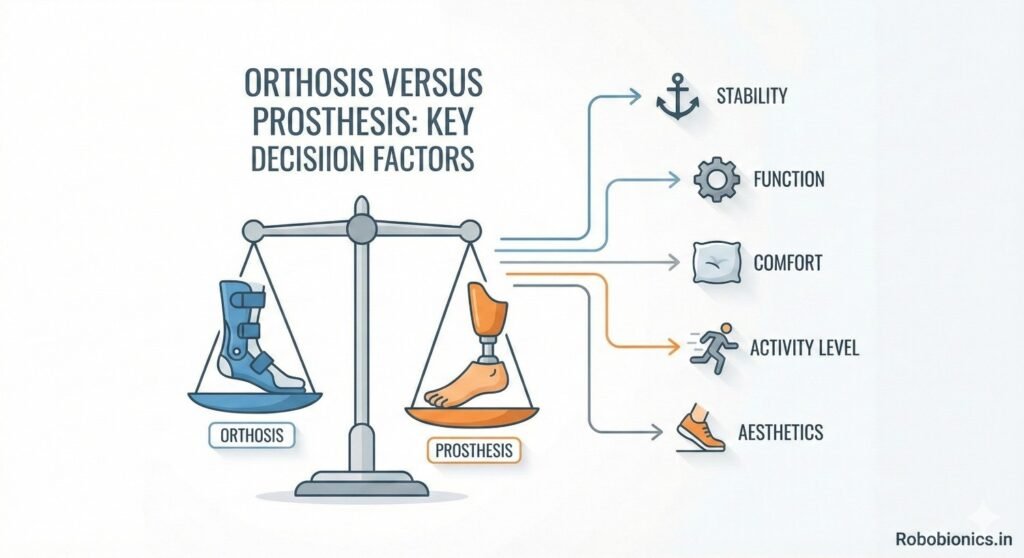
Foot length is one of the strongest indicators.
More remaining length favors orthoses.
Less length favors prostheses.
Doctors should assess effective lever arm, not just appearance.
Functional testing clarifies this.
Visual assessment alone is misleading.
This factor must be considered early.
Delays increase compensations.
Timely decisions improve adaptation.
Patients with reduced sensation need careful load control.
Orthoses may create hidden pressure points.
Prostheses may distribute load more evenly.
Tissue quality affects tolerance.
Fragile skin requires protective solutions.
Device choice must prioritize safety.
Regular skin inspection is essential.
Education supports early detection.
Prevention is better than treatment.
Active patients with good balance may manage with orthoses longer.
Lower activity patients may benefit from prostheses earlier.
Endurance matters.
Balance deficits favor prosthetic stability.
Orthoses rely on neuromuscular control.
Assessment must be honest.
Activity goals guide decisions.
Daily walking demands should be realistic.
Device choice must match lifestyle.
Watching how a patient walks without support provides valuable information.
Subtle limping, shortened steps, or early heel rise often indicate loss of forefoot leverage.
These signs may appear even when the patient reports feeling fine.
Doctors should observe walking on flat ground and during turns.
Difficulty controlling speed or stopping smoothly is important.
These findings often predict long-term issues.
Barefoot observation should be brief and safe.
It is not for endurance testing.
It simply reveals natural compensation patterns.
Temporary fillers or trial orthoses can clarify needs.
Improved stability with support suggests benefit from a device.
Lack of improvement signals need for a different approach.
Patients often feel the difference immediately.
This feedback is valuable.
It helps guide shared decisions.
Short trials reduce guesswork.
They allow real-world observation.
Clinical confidence improves.
Partial foot loss increases energy cost during walking.
This may not be obvious in short distances.
Longer observation reveals fatigue patterns.
Patients may slow down or rely more on the intact side.
These changes stress other joints.
Early detection prevents secondary pain.
Energy efficiency is a key goal.
Devices should reduce effort, not add to it.
Gait analysis supports this aim.
Unprotected partial foot amputations often develop ulcers.
Pressure shifts to areas not designed to bear weight.
This is common in diabetic patients.
Ulcers may start small and painless.
They worsen quickly if unnoticed.
Delayed intervention increases infection risk.
Proper device choice reduces pressure peaks.
Both orthoses and prostheses can help when chosen correctly.
Prevention is always preferable.
Compensatory walking patterns strain joints over time.
Knees, hips, and the lower back are most affected.
Pain often appears months after amputation.
Patients may not connect joint pain to foot loss.
This delays appropriate treatment.
Early support prevents this cascade.
Reducing asymmetry protects the entire body.
Device choice has long-term implications.
Whole-body health must be considered.
Instability and fatigue reduce confidence.
Patients begin limiting activity to avoid discomfort.
This leads to deconditioning.
Reduced activity worsens balance and strength.
The problem compounds itself.
Timely support breaks this cycle.
Devices should encourage movement, not restrict it.
Comfort and stability restore confidence.
This supports independence.
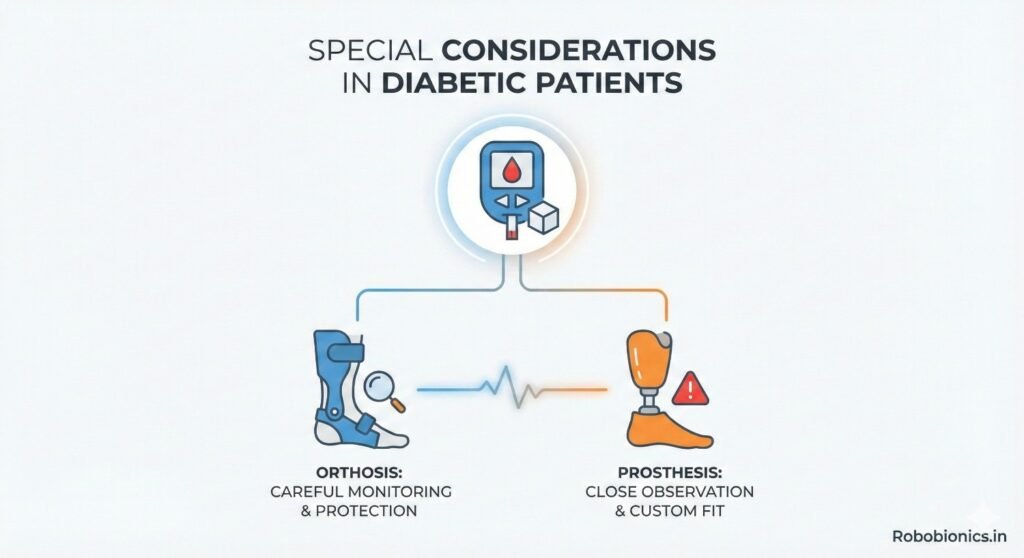
Many diabetic patients have reduced foot sensation.
They may not feel pressure or injury.
This increases risk with poorly fitted devices.
Orthoses must be carefully designed and monitored.
Prostheses may offer better load distribution.
Frequent follow-up is essential.
Education on daily skin checks is critical.
Patients must understand warning signs.
Support systems matter.
Poor blood flow affects healing and tolerance.
Skin may break down easily.
Device-induced pressure must be minimized.
Doctors should assess vascular status before deciding.
Healing capacity guides aggressiveness of intervention.
Safety must guide choice.
Sometimes simpler solutions are safer initially.
Progression may be gradual.
Flexibility improves outcomes.
Inadequate support increases risk of further tissue loss.
Repeated ulcers may lead to higher-level amputation.
This is a serious consequence.
Choosing the right device early reduces this risk.
Protecting remaining tissue is paramount.
Long-term thinking is essential.
Footwear plays a major role in device success.
Orthoses rely on proper shoes for effectiveness.
Poor footwear limits benefit.
Prostheses may require custom shoes or inserts.
Patients must be willing to adapt.
Lifestyle compatibility matters.
Doctors should discuss footwear early.
Surprises reduce compliance.
Preparation improves acceptance.
Patients who stand or walk for long periods need durable solutions.
Orthoses may fatigue faster under heavy use.
Prostheses often provide better endurance.
Work surfaces also matter.
Uneven ground increases instability.
Device choice must reflect environment.
Activity goals should be realistic.
Overambition leads to disappointment.
Honest planning supports success.
Some patients worry about appearance.
Bulky devices may cause resistance.
This affects daily use.
Doctors should acknowledge these concerns.
Education and design options help.
Acceptance improves with understanding.
Comfort and function usually outweigh cosmetic issues over time.
Early reassurance helps patients adapt.
Respectful discussion matters.
Orthotic solutions may work initially but fail over time.
Increasing fatigue, pain, or instability are warning signs.
These should prompt reassessment.
Doctors should not view transition as failure.
It reflects changing needs.
Adaptation is part of care.
Early recognition prevents prolonged discomfort.
Patients progress faster with the right support.
Timely transition improves outcomes.
Patients may resist moving to a prosthesis.
Fear of complexity or stigma is common.
Education reduces anxiety.
Explaining functional benefits helps.
Demonstrations can be effective.
Seeing improvement builds confidence.
Gradual transition plans work best.
Patients feel supported.
Trust is preserved.
Before transitioning, reassessment is essential.
Strength, balance, and skin health should be reviewed.
Goals may need adjustment.
Prosthetic trials can clarify benefit.
Temporary fittings provide insight.
Patient feedback is valuable.
Reassessment ensures readiness.
Safety remains the priority.
Structured planning supports success.
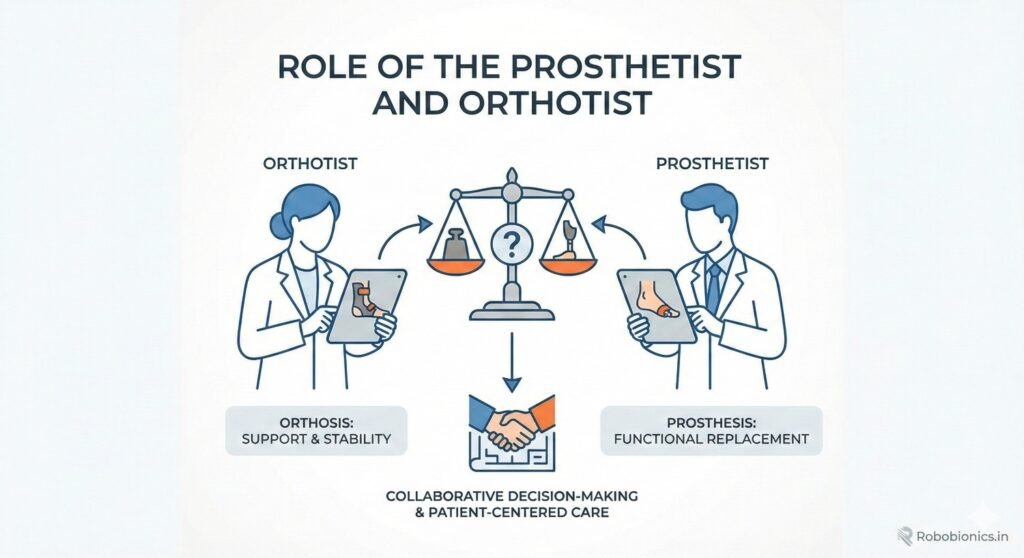
Choosing between prosthesis and orthosis requires teamwork.
Doctors, prosthetists, and therapists each bring expertise.
Collaboration improves decisions.
Shared assessment reduces bias.
Different perspectives highlight different risks.
Unified plans support patients better.
Patients benefit from coordinated messaging.
Conflicting advice undermines trust.
Team alignment is essential.
Generic solutions rarely work well.
Partial foot loss varies widely.
Customization improves comfort and function.
Both orthoses and prostheses require precise design.
Small adjustments make big differences.
Attention to detail matters.
Ongoing refinement is normal.
Devices evolve with patient needs.
Flexibility supports long-term use.
Patients need education on use and care.
Daily inspection and maintenance are critical.
Neglect leads to complications.
Regular follow-up detects issues early.
Adjustments prevent breakdown.
Long-term success depends on monitoring.
Providers must emphasize this commitment.
Care does not end at fitting.
Support is ongoing.
Proper device choice improves mobility significantly.
Patients walk more confidently and efficiently.
Independence increases.
Confidence encourages activity.
Activity supports overall health.
This creates positive momentum.
Poor choices limit potential.
Patients may withdraw.
Correct decisions unlock capability.
Supporting the foot properly protects the whole body.
Joint pain and back issues are reduced.
Energy efficiency improves.
Preventing ulcers avoids hospitalizations.
Quality of life improves.
Healthcare costs decrease.
Early investment in the right device pays off.
Long-term benefits are substantial.
Prevention is powerful.
Feeling stable restores confidence.
Patients worry less about falling.
Mental stress decreases.
Independence supports self-esteem.
Patients feel more in control.
This improves overall outlook.
Device choice affects more than movement.
It affects identity and confidence.
Holistic care matters.
Partial foot and toe amputations require careful attention, even when they appear minor.
The decision between a prosthesis and an orthosis must be based on function, not assumptions or convenience.
Foot length, stability, skin health, and activity demands all play crucial roles.
At Robobionics, our experience shows that early, thoughtful intervention prevents many long-term problems.
Neither prostheses nor orthoses are universally better.
The right choice depends on the individual and may change over time.
When clinicians and patients work together to evaluate real-world function, outcomes improve.
Comfort, safety, and confidence become achievable goals.
The best solution is the one that supports stable, pain-free movement for the long term.

For many clinicians, the surgery is only the first step. What happens after the operation
For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much
Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.