
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation

Before a prosthetic socket is made, the skin tells a story.
It shows pain, healing, pressure, risk, and readiness. Many problems with prosthetic comfort, fit, and long-term use begin before the socket is ever cast. They begin with skin that was not fully ready, not carefully checked, or not respected enough.
As prosthetics manufacturers with years of hands-on experience across India, we have seen this again and again. A socket may look perfect on paper, but if the skin underneath is weak, irritated, or damaged, failure is only a matter of time. Pain follows. So does loss of confidence. Sometimes, the user gives up altogether.
This is why skin integrity monitoring before socket casting is not optional. It is essential. It is the job of the physician, prosthetist, and care team to pause, look closely, and act early.
In this article, we will walk through the key physician red flags that must never be ignored before socket casting. We will explain what to look for, why it matters, and what actions should be taken. No complex terms. No theory-heavy talk. Only practical, real-world guidance drawn from years of clinical and manufacturing experience.
Because when skin is protected, outcomes improve.
And when outcomes improve, lives truly change.
The prosthetic socket sits directly on the skin for many hours every day.
There is no buffer, no margin for error, and no place to hide problems once the socket is made.
If the skin is already weak, dry, swollen, or injured, the socket will only make things worse.
Pressure increases. Heat builds up. Friction rises.
Over time, small issues turn into pain, wounds, and infections.
This is why skin condition must always be checked before casting, not after problems begin.
Many people believe that a better socket design will solve skin pain.
This is not fully true.
A socket can only work well if the skin is healthy enough to accept load.
If the base is weak, even the best design will fail.
Physicians play a key role here.
They must identify risks early and delay casting when needed, even if the patient is eager to move ahead.
Skipping skin checks may seem faster in the short term.
But it often leads to repeated fittings, long breaks from prosthetic use, and high emotional stress.
When skin is respected early, the entire prosthetic journey becomes smoother.
Fewer revisions. Better comfort. Higher trust.

Skin assessment is not just about looking at the limb from a distance.
It requires time, touch, and careful questioning.
The physician must observe color, temperature, texture, and response to pressure.
Each of these gives clues about how the skin will behave inside a socket.
Ignoring these signs is one of the most common reasons for early socket failure.
Patients often describe burning, itching, tightness, or deep pain.
These symptoms may not always show clearly on the skin surface.
A good physician listens closely and treats these words as early warnings.
Pain described before casting usually becomes worse after socket use.
Trusting patient feedback is just as important as clinical findings.
Skin care before casting is a team effort.
Physicians, prosthetists, and therapists must share observations openly.
When everyone works together, decisions become safer and more patient-focused.
When communication breaks down, the skin often pays the price.
Any open wound, even a small one, is a clear reason to delay socket casting.
Sockets create constant pressure and friction that prevent healing.
What looks minor today can turn into a deep ulcer within days of socket use.
This is especially risky for people with poor circulation or nerve damage.
Casting over open skin is never worth the risk.
Scars may look healed but still be fragile underneath.
Some scars tear easily, while others become painful under pressure.
Hard, shiny, or tight scars often do not stretch well.
When placed inside a socket, they break down faster than normal skin.
Physicians should gently press and move scar tissue to test its strength.
If wounds or weak scars are found, casting must be postponed.
The focus should shift to healing, skin care, and protection.
Simple steps like proper dressing, massage, and rest can improve skin quality.
Only when the skin is truly stable should socket casting be planned.
Some redness after activity is normal.
Healthy skin returns to its normal color within a short time.
Warning redness stays for long periods and may feel warm or painful.
This shows that the skin is already under stress.
If redness remains after light pressure, it is a sign the skin is not ready.
Long-lasting redness often points to poor blood flow or early inflammation.
These conditions reduce the skin’s ability to handle pressure.
Inside a socket, this redness can quickly turn into blisters or wounds.
The problem grows silently until pain becomes severe.
Physicians should treat persistent redness as a serious alert.
When redness does not fade, casting should be delayed.
The cause must be identified and treated first.
Rest, skin cooling, and circulation support may be needed.
Rushing forward only increases the risk of long-term damage.
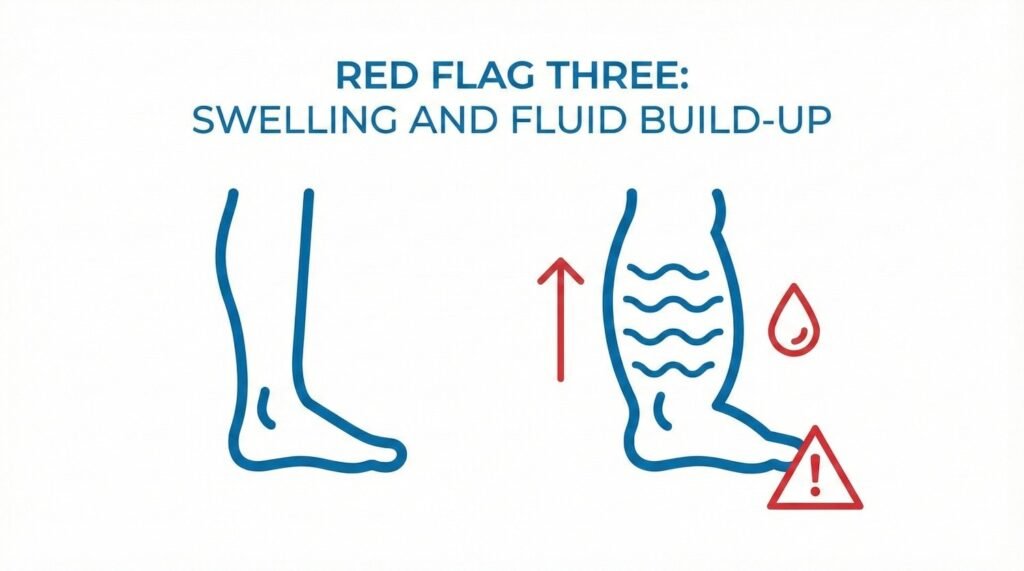
Swelling changes the shape and size of the limb.
A socket made on a swollen limb will not fit once swelling reduces.
This leads to looseness, movement, and uneven pressure.
All of these harm the skin and reduce control.
Stable limb size is essential for safe socket casting.
Swollen skin is stretched and fragile.
It breaks down faster under pressure and heat.
Fluid build-up also reduces oxygen supply to skin tissues.
This slows healing and increases infection risk.
Even mild swelling should be taken seriously.
Before casting, swelling must be controlled.
This may include compression, elevation, or medical treatment.
Once limb size remains stable over time, casting becomes safer.
Patience at this stage prevents many future problems.
Dry skin may not seem dangerous, but it is less flexible and more prone to injury.
Cracks allow bacteria to enter and cause infection.
Inside a socket, dry skin experiences constant rubbing.
This makes cracks deeper and more painful over time.
Healthy skin needs moisture to stay strong.
Dryness can come from poor hygiene, harsh soaps, or low blood flow.
In some cases, it points to deeper medical issues.
Physicians should not ignore dry skin as a minor issue.
It often signals that the skin barrier is already damaged.
Understanding the cause helps guide proper care.
Moisturizing routines should begin before casting.
Simple creams used regularly can improve skin quality.
Patients should be taught gentle cleaning and drying habits.
Only when the skin feels soft and intact should socket casting move ahead.
Skin that hurts with light touch is not ready for load.
This pain often points to nerve irritation or deep tissue stress.
Inside a socket, this pain will multiply quickly.
What starts as discomfort becomes unbearable pressure.
Pain should never be ignored in pre-casting checks.
Some sensitivity after surgery is expected.
However, sharp, burning, or electric pain is not normal.
These pain types suggest nerve involvement or inflammation.
Sockets can worsen these conditions if applied too soon.
Physicians must take time to understand pain patterns.
When pain is present, the focus should shift to treatment.
Medication, rest, or therapy may be needed first.
Delaying casting is not a setback.
It is a step toward long-term comfort and success.
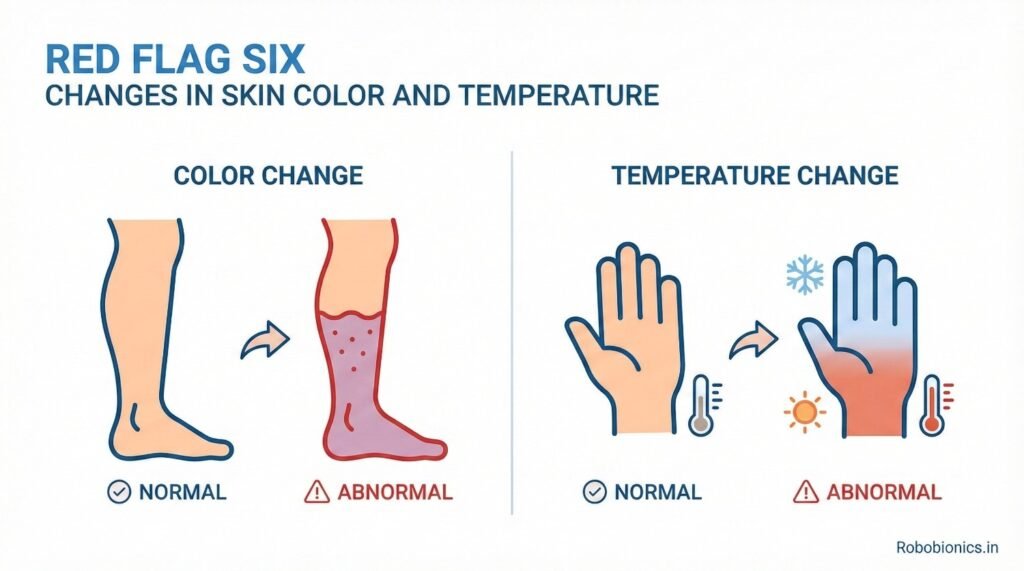
Skin color gives strong signals about blood flow and tissue health, especially in an amputated limb that will soon carry prosthetic load for many hours every day.
Pale, bluish, or darkened skin often points to poor circulation, while uneven patches may show areas that cannot handle pressure well.
These color changes may not always cause pain, but they show that the skin is already under stress.
If ignored, these areas often become the first points of breakdown inside a socket.
Physicians must compare both limbs and note even mild differences, as small changes often predict larger problems later.
Healthy skin usually feels warm and balanced when touched.
Cold skin can signal low blood flow, while excessive warmth may indicate inflammation or infection.
When a limb shows uneven temperature zones, it means the tissues are not responding evenly to pressure.
Inside a socket, this uneven response leads to pressure peaks that damage skin quickly.
Temperature checks should always be part of pre-casting assessment, not an afterthought.
If color or temperature changes are present, casting should not be rushed.
Further tests or circulation support may be required before moving ahead.
Addressing these issues early gives the skin a chance to recover and adapt.
This approach protects both the patient’s comfort and the long-term success of the prosthesis.
A history of ulcers, blisters, or repeated skin wounds is one of the strongest warning signs before socket casting.
Skin that has broken down before is more likely to fail again under pressure.
Even if the skin looks healed, the tissue underneath may still be weak.
Scarred or previously injured areas rarely tolerate load the same way as healthy skin.
Physicians must always ask about past skin issues and document them carefully.
It is not enough to know that a wound occurred.
The reason behind it matters just as much.
Poor fit, long wear time, moisture build-up, or poor sensation can all lead to breakdown.
If these causes are not addressed, the same cycle will repeat with a new socket.
A clear understanding helps guide safer socket design and timing.
When past breakdown is known, extra caution is required before casting.
Skin preparation, gradual loading, and close follow-up become essential.
In some cases, delaying casting until skin strength improves is the safest choice.
This delay often saves months of pain and repeated adjustments later.
Sensation allows the body to warn the user when pressure becomes harmful.
When sensation is reduced, these warning signs are lost.
Numb skin can be damaged without the patient realizing it.
By the time pain appears, the injury is often already severe.
This makes sensory checks a critical part of pre-casting evaluation.
Nerve injury, diabetes, and long-term swelling can all reduce sensation.
Some patients may not even realize their feeling has changed.
Simple touch tests can reveal areas of numbness.
Physicians should test lightly and ask patients to describe what they feel.
Any loss of sensation increases the risk of silent skin injury.
When sensation is poor, socket casting must be planned very carefully.
Extra padding, pressure relief, and slow break-in schedules become essential.
In some cases, additional skin conditioning or monitoring tools may be needed.
Protecting numb skin requires planning, patience, and clear patient education.
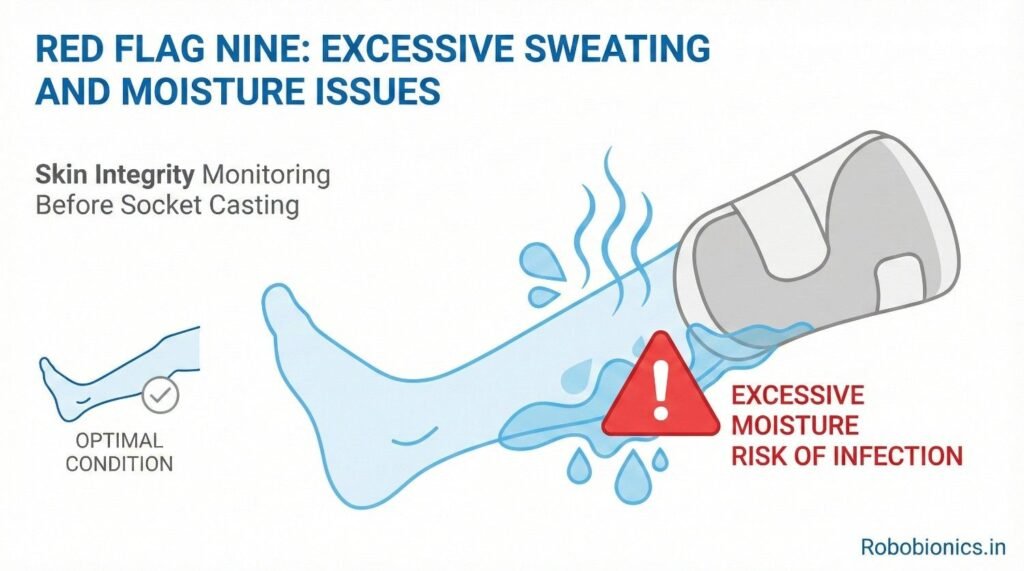
Skin that stays damp for long periods becomes soft and fragile.
It breaks down faster under pressure and friction.
Inside a prosthetic socket, sweat has nowhere to escape.
This creates a warm, wet environment that damages skin quickly.
Excessive sweating before casting is a clear risk factor.
Sweating may increase due to anxiety, climate, or poor skin care habits.
In some cases, it is linked to nerve changes or medication use.
Physicians should ask targeted questions and observe moisture levels during exams.
Ignoring sweating issues often leads to repeated skin complaints later.
Understanding the cause allows better planning and prevention.
Before moving ahead with socket casting, moisture control strategies should be in place.
This may include skin care routines, breathable liners, or gradual wear plans.
Patients should be taught how to keep the skin clean and dry throughout the day.
When moisture is controlled early, skin health improves significantly.
Clean skin resists infection and heals faster.
Poor hygiene increases bacteria load and weakens the skin barrier.
If a patient struggles with daily skin care, problems will appear inside the socket.
This is not a judgment, but a reality that must be addressed early.
Physicians should assess hygiene ability with care and respect.
Some patients lack access to clean water, proper supplies, or education.
Others may have physical limits that make daily care difficult.
These challenges must be discussed openly and without criticism.
Only then can real solutions be found.
Ignoring these barriers puts the skin at constant risk.
Before casting, patients should receive clear guidance on skin care routines.
Simple steps, explained well, often make a big difference.
When patients feel supported rather than judged, they follow care plans better.
This support protects skin health and improves prosthetic outcomes.
Stress affects the body in many ways, including skin health.
High stress can increase sweating, reduce healing, and lower pain tolerance.
Patients under emotional strain may ignore early skin warning signs.
They may push through pain to avoid delays.
Physicians must recognize this risk and address it gently.
Strong desire to walk or use a hand again is natural and positive.
However, when urgency overrides safety, skin often suffers.
Patients may hide pain or discomfort to speed up the process.
This honesty gap can lead to serious skin injury.
Open conversations help balance hope with safety.
Physicians should reassure patients that delays are part of good care, not failure.
Clear explanations build trust and reduce pressure.
When patients understand the reasons behind caution, cooperation improves.
This shared understanding protects skin and long-term function.
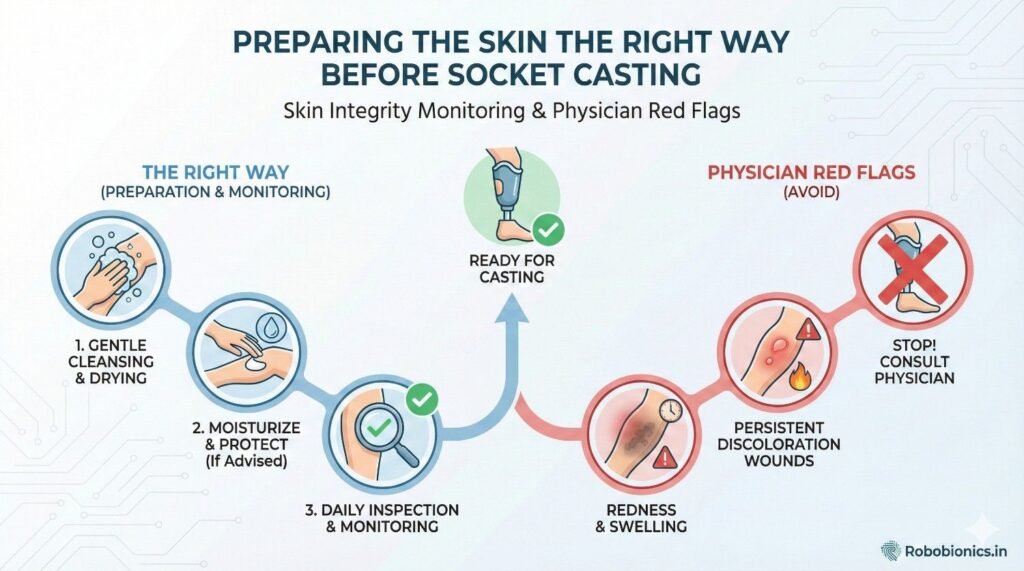
Skin preparation before socket casting should never be treated as a routine step that is completed quickly just to move the process forward.
It is a medical decision that directly affects comfort, safety, and long-term prosthetic use.
When skin is prepared well, the socket works with the body instead of fighting it.
When skin is ignored, even small issues can grow into serious setbacks.
Physicians must treat this stage with the same seriousness as surgery or rehabilitation planning.
After amputation or injury, skin goes through many changes as it heals and adjusts to new demands.
It needs time to become stronger, more flexible, and more tolerant of pressure.
Casting too early often locks in problems that cannot be corrected later without major changes.
Waiting until the skin shows stable behavior is not delay, it is good practice.
Patience at this stage often leads to faster success later.
Skin readiness should be based on clear signs, not assumptions or timelines.
Stable color, controlled swelling, intact surface, and manageable sensitivity are all essential markers.
Physicians should document these signs and review them carefully before approving casting.
Clear criteria remove guesswork and protect both the patient and the care team.
Many patients do not fully understand how skin health affects prosthetic success.
They may see skin issues as minor or temporary compared to limb loss.
Without proper explanation, they may push for casting too soon.
This pressure can lead to poor decisions and avoidable pain.
Clear, calm communication helps patients see the bigger picture.
Medical language often creates confusion or fear.
Using simple words helps patients truly understand what is at stake.
Explaining how pressure, heat, and friction affect weak skin builds awareness.
When patients understand cause and effect, they cooperate more willingly.
This shared understanding builds trust and reduces frustration.
Patients must feel safe reporting pain, itching, or discomfort without fear of delay or judgment.
If they hide symptoms, skin damage often follows.
Physicians should ask open questions and listen carefully.
A few extra minutes of conversation can prevent months of trouble.
Honest feedback is one of the strongest tools in skin protection.
Every patient heals at a different pace based on age, health, and lifestyle.
Using fixed timelines for casting often leads to poor outcomes.
Skin may look healed on the surface while still being weak underneath.
Only careful assessment reveals true readiness.
Physicians must resist pressure to follow schedules instead of skin signals.
One good skin check is not always enough.
Stability over days or weeks gives a clearer picture.
Skin that remains calm under light activity is more likely to tolerate a socket.
Skin that changes daily is still adjusting and needs more time.
Repeated checks improve decision accuracy.
Casting should support rehabilitation, not interrupt it.
If skin breaks down early, therapy is often paused or slowed.
When timing is aligned correctly, patients progress more smoothly.
They build confidence instead of facing repeated setbacks.
Good timing protects both physical and emotional recovery.
Ignoring skin warnings often leads to wounds, infections, and severe pain.
These issues can force long breaks from prosthetic use.
Repeated injuries weaken the skin further and reduce tolerance over time.
Some patients never regain full confidence in their prosthesis.
These outcomes are often preventable with early caution.
Skin failure affects more than the body.
It damages trust, motivation, and self-belief.
Patients may feel that the prosthesis is not meant for them.
They may withdraw from therapy or daily activities.
Protecting skin early helps protect emotional health as well.
Skin-related complications increase clinic visits, adjustments, and remakes.
They raise costs for patients, providers, and health systems.
Time spent fixing preventable issues could be used for progress instead.
Good skin assessment is both humane and efficient.

In busy clinical settings, speed often becomes the priority.
However, faster is not always better in prosthetic care.
A skin-first approach values readiness over timelines.
It encourages careful decisions instead of rushed outcomes.
This shift improves results for everyone involved.
All members of the care team should understand skin risks and red flags.
Shared knowledge leads to shared responsibility.
Regular discussions and case reviews help reinforce good habits.
Learning from past complications strengthens future care.
Education is a powerful tool in prevention.
Patients who understand their skin become active partners in care.
They notice changes early and report them promptly.
Simple education builds confidence and responsibility.
Empowered patients protect their own outcomes.
This partnership is key to long-term success.
Refusing to cast when skin is not ready can feel difficult.
Patients may be disappointed or frustrated.
However, saying no at the right time prevents greater harm later.
It shows commitment to safety and quality.
A thoughtful delay is often the most caring choice.
Delays should always come with a clear plan.
Patients need to know what steps will move them forward.
Skin care routines, timelines, and follow-ups should be explained clearly.
This reduces anxiety and keeps motivation strong.
Support turns delay into progress.
When skin becomes stable, calm, and resilient, casting feels different.
The limb responds well to touch and pressure.
This readiness leads to better fit and comfort from the start.
The difference is noticeable to both patient and clinician.
Waiting for this moment is worth it.
Skin assessment works best when the patient feels calm, respected, and unhurried, because stress and fear often change how the skin behaves and how honestly symptoms are shared.
A rushed exam may miss small but important signs that only appear when the patient relaxes and speaks freely.
Physicians should explain each step before touching the limb, so the patient understands what is being checked and why it matters.
This approach builds trust and leads to more accurate findings.
A calm setting allows both the skin and the patient’s story to speak clearly.
Good skin checks cannot rely on sight alone, because many risks lie beneath the surface.
Gentle pressure, light touch, and slow movement reveal how the skin responds under stress.
Physicians should take time to feel temperature changes, firmness, and sensitivity across different areas of the limb.
Each region may behave differently and needs individual attention.
Time spent here often prevents months of future problems.
Patients may not volunteer skin concerns unless asked directly.
Simple, open questions often uncover hidden issues.
Asking about pain after activity, itching at night, or past wounds helps reveal risk patterns.
The tone should always be supportive, not interrogative.
When patients feel heard, they share more honestly.
Clear records help guide decisions and protect both patient and provider.
They show why casting was delayed or approved.
Skin findings change over time, and memory alone is unreliable.
Written notes allow comparison across visits.
Good documentation supports safe, consistent care.
Notes should include color changes, swelling levels, pain reports, and scar condition.
Even mild issues should be recorded.
Photos, when allowed, can also help track progress.
They offer objective reference points for future decisions.
Small details often matter the most later.
Shared documentation allows prosthetists and therapists to plan better.
Everyone works from the same understanding.
This reduces miscommunication and repeated mistakes.
It also builds confidence across the care team.
Clear records lead to clear actions.
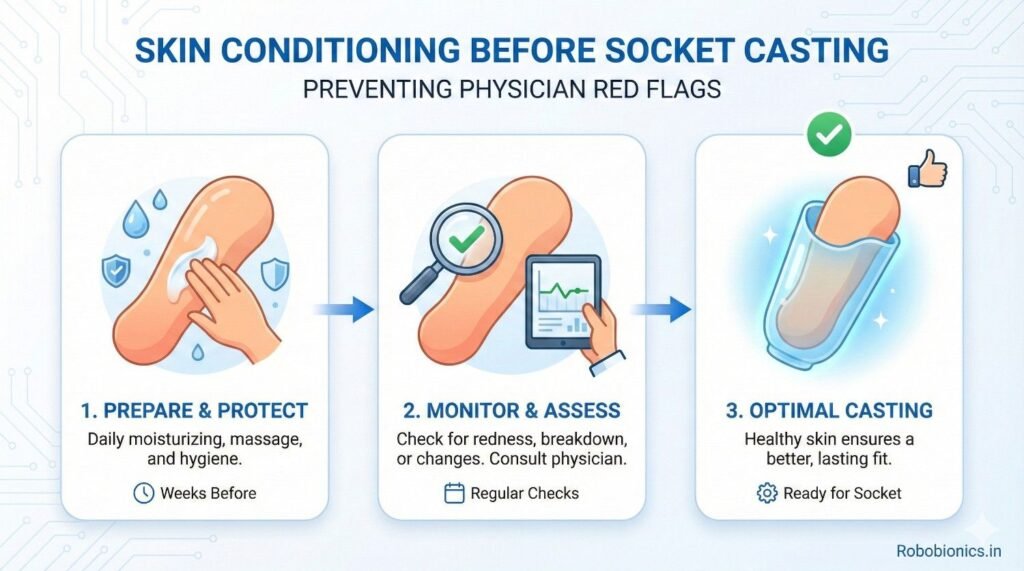
Skin can be trained to tolerate pressure when done slowly and safely.
This process prepares the limb for socket use.
Gentle massage, light compression, and controlled activity help improve circulation and strength.
These steps must be guided and monitored.
Rushing conditioning often does more harm than good.
Patients should learn basic skin care routines they can follow at home.
These routines should be realistic and easy to maintain.
Cleaning, drying, moisturizing, and checking the skin daily builds strong habits.
Consistency matters more than complexity.
Simple actions repeated daily create lasting protection.
Conditioning should continue until the skin responds calmly to pressure and activity.
Redness should fade quickly and pain should remain mild or absent.
Once these signs are stable, casting becomes safer.
Stopping too early increases risk.
Patience here pays off later.
These patients often have reduced healing ability and weaker skin.
Even small injuries can become serious quickly.
Physicians must be extra cautious and conservative with timelines.
More frequent checks are often needed.
Protecting skin in these cases requires strict attention and teamwork.
Aging skin is thinner and tears more easily.
It also recovers more slowly from stress.
Socket casting for elderly patients should only proceed when skin is clearly stable.
Extra padding and careful design may be required.
Gentle handling is essential at every step.
When feeling is reduced, the skin cannot warn the patient about danger.
This makes early detection harder.
Physicians should plan for closer follow-up and education.
Patients must be taught to rely on visual checks instead of pain.
Safety depends on awareness and routine.
Skin assessment does not end with the physician.
Prosthetists must use this information to guide socket design.
Areas of risk should receive relief, not pressure.
Strong areas should carry more load.
Good design starts with good skin information.
Even when skin looks ready, care must be taken during casting itself.
Positioning, pressure, and timing all matter.
Rough handling can undo weeks of preparation.
Casting should always be gentle and controlled.
Respect for skin continues through every step.
First fittings are critical for skin safety.
Early checks catch problems before they grow.
Prosthetists and physicians should plan follow-up together.
Quick response prevents long-term damage.
Skin protection is an ongoing process.
Patients should know what healthy skin looks and feels like inside a socket.
This knowledge helps them spot problems early.
Redness that fades, mild warmth, and even pressure are usually normal.
Pain, open skin, or lasting marks are not.
Clear examples help patients act quickly.
Daily skin checks should become a habit, not a chore.
Patients should inspect all areas carefully.
Mirrors, phone cameras, or family support can help.
No area should be ignored.
Early action prevents serious injury.
Patients must feel safe reporting issues without fear of blame.
Problems should be seen as shared challenges, not failures.
When reporting is encouraged, outcomes improve.
Silence only leads to harm.
Open communication protects everyone.

For many years, skin problems in prosthetic users have been treated only after they appear.
Pain is reported, wounds are seen, and then action is taken.
This reactive approach costs time, comfort, and trust.
By the time the problem is visible, damage is often already done.
A preventive mindset, where skin integrity is checked deeply before socket casting, changes everything.
It stops problems before they begin.
Skin is not just a covering.
It is a living system that reacts to pressure, heat, emotion, and health.
When skin is respected, it adapts and grows stronger.
When it is ignored, it fails quietly and suddenly.
Physicians who treat skin as a priority create safer and more lasting outcomes.
This respect shows in every decision they make.
Skin integrity standards should not change from one clinic to another.
Patients deserve the same level of care everywhere.
Clear protocols, shared language, and team alignment help achieve this.
When everyone follows the same principles, outcomes improve across the board.
Consistency builds confidence for both patients and professionals.
As prosthetics manufacturers working closely with clinics across India, we have seen one clear pattern.
When skin checks are rushed or ignored, failure follows.
We have also seen the opposite.
When physicians slow down, ask the right questions, and delay casting when needed, success rates rise sharply.
These lessons are not theoretical.
They are based on real people, real limbs, and real outcomes.
A single decision to wait one more week for skin to stabilize can prevent months of pain.
A simple conversation about dryness or redness can avoid repeated socket changes.
These small choices often separate good outcomes from poor ones.
They require awareness, not advanced tools.
Good care is built on attention, not speed.
Patients may forget technical details, but they never forget pain.
They also never forget when a clinician protected them from harm.
When skin is protected, trust grows naturally.
This trust improves cooperation, follow-up, and long-term use.
Skin safety is not just clinical care.
It is relationship building.
No socket, no matter how advanced, can succeed on unhealthy skin.
Technology cannot replace basic biological readiness.
Physician red flags exist for a reason.
They are early warnings that ask for attention, not delay.
Ignoring them leads to predictable failure.
Respecting them leads to lasting success.
Many patients fear delay more than damage.
It is the physician’s role to reframe this thinking.
Waiting for skin readiness protects mobility, confidence, and independence.
It saves patients from repeated pain and disappointment.
A delayed cast done right is better than a rushed cast done early.
At its core, prosthetic care is about restoring dignity and function.
This cannot happen if skin health is compromised.
By making skin integrity monitoring a strict standard before socket casting, physicians protect what matters most.
Comfort. Safety. Trust. Long-term use.
When skin is cared for first, everything else follows.

For many clinicians, the surgery is only the first step. What happens after the operation
For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much
Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.