
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
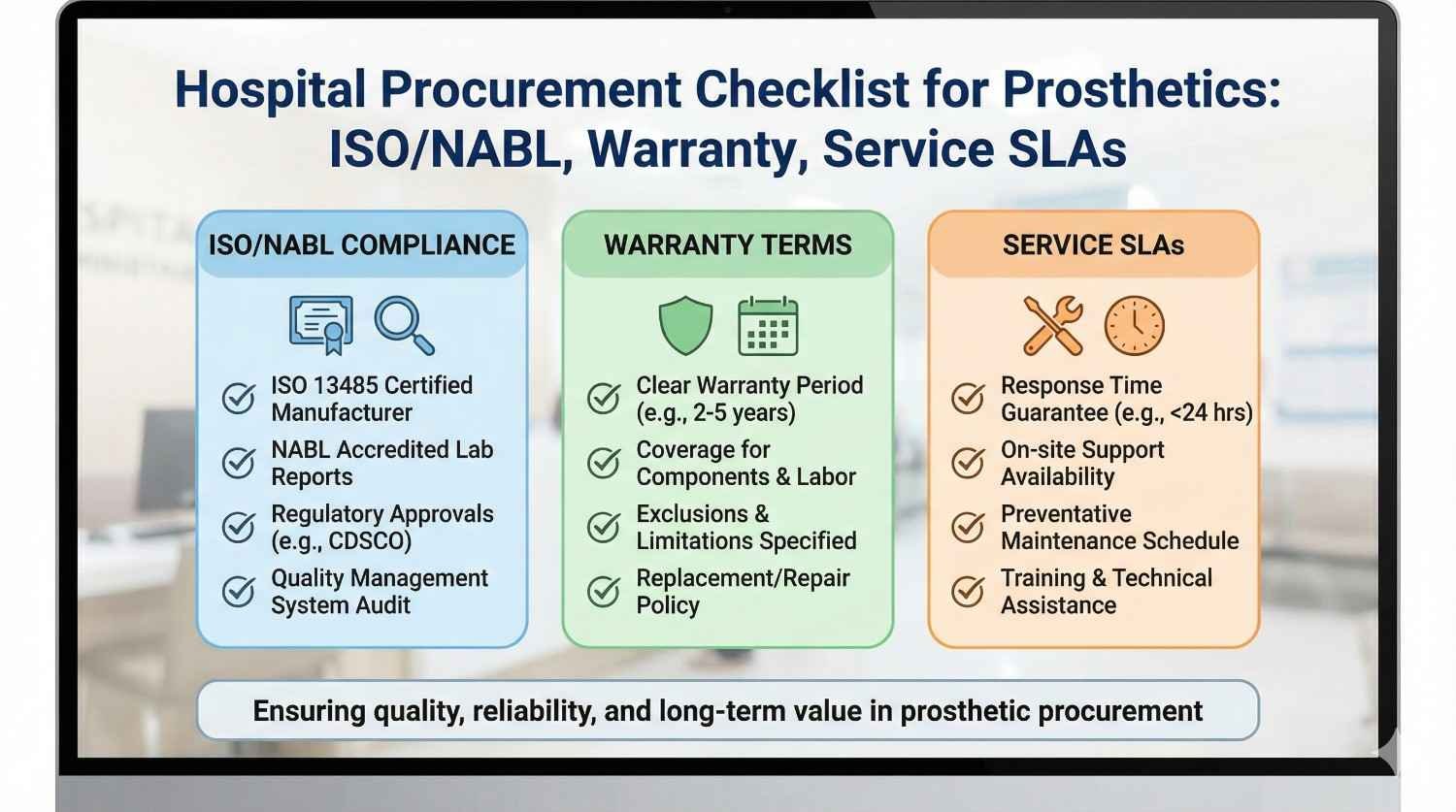
Hospital procurement teams carry a quiet but heavy responsibility. The prosthetic you approve today will shape a patient’s safety, comfort, and independence for years. Yet procurement decisions are often rushed, price-led, or based on incomplete checklists. This guide is written to change that. In simple words, it walks hospitals through what truly matters when procuring prosthetics in India—certifications, quality systems, warranties, service commitments, and long-term accountability—so decisions are safe, defensible, and patient-first.
Most medical devices remain inside hospital walls.
Prosthetics leave the hospital and become part of a patient’s daily life.
This changes responsibility completely.
Failure happens at home, at work, or on the road, not in a ward.
Procurement must think beyond delivery.
Long-term use is the real test.
A prosthesis is never finished on the day it is issued.
Fit changes, usage increases, and problems appear over time.
Without service support, even a good product fails.
Procurement must evaluate the service system behind the device.
This makes vendor capability as important as hardware quality.
Ignoring this leads to repeat failures.
When a prosthesis fails, patients return to the hospital.
Complaints, audits, and legal questions often follow.
Procurement decisions are reviewed closely in such cases.
Documentation and due diligence become critical.
A strong checklist protects the hospital.
It also protects patients.

ISO certification shows that a vendor follows a documented quality system.
It does not mean the product is perfect, but that processes are controlled.
For hospitals, this reduces variability risk.
It ensures repeatability and traceability.
ISO matters most when issues arise.
It shows systems exist to correct them.
ISO 13485 is specific to medical devices.
It covers design, manufacturing, and post-market processes.
For prosthetics, this certification is critical.
It shows the vendor understands medical risk management.
Hospitals should prefer vendors with ISO 13485.
It aligns with global best practice.
Some vendors show ISO certificates without scope clarity.
The certificate may not cover prosthetics.
Procurement teams should verify scope and validity.
A quick check prevents future trouble.
Certificates should be current and verifiable.
Old or vague documents are a warning sign.
NABL accreditation applies to testing and calibration labs.
It becomes relevant when mechanical or electrical testing is involved.
For bionic or powered prosthetics, testing credibility matters.
It supports safety and performance claims.
Hospitals should ask where testing is done.
Accredited labs add confidence.
Some vendors test in-house.
Others rely on external labs.
In-house testing is acceptable if systems are strong.
Third-party NABL labs add independent validation.
Procurement should understand both models.
Transparency is more important than location.
Test reports should be readable and relevant.
Generic reports add little value.
Hospitals should look for test purpose and limits.
Reports must link to real-world use.
Asking basic questions reveals quality.
Good vendors explain clearly.
A prosthesis may pass all lab tests and still fail users.
Daily life is harsher than controlled environments.
Hospitals should ask for field performance data.
This shows how devices behave in real conditions.
Clinical use history matters.
It reduces uncertainty.
Hospitals do not need academic trials for every device.
But usage data, case summaries, and outcomes help.
Evidence should reflect Indian conditions.
Climate, terrain, and user activity matter.
Local data is more useful than foreign brochures.
Context matters.
Marketing language often exaggerates capability.
Procurement should ask for examples, not promises.
A simple question like “where is this used” reveals much.
Real answers build trust.
Vendors who avoid specifics raise concern.
Evidence should speak.

A long warranty sounds attractive.
But coverage details matter more than duration.
Some warranties exclude key components.
Others limit usage conditions.
Hospitals must read what is actually covered.
Fine print decides value.
Warranty should clearly state parts and labor inclusion.
Ambiguity causes disputes.
Response timelines should be written, not implied.
Delays hurt patients and hospitals.
Clear terms reduce friction.
They protect all sides.
Liners, gloves, and cosmetic covers wear out.
Most warranties exclude them.
Hospitals should understand these exclusions.
Patients should be informed early.
Transparency prevents complaints later.
Expectation setting is part of care.
Service delays directly affect mobility and dignity.
A broken prosthesis is an emergency for the user.
Hospitals must ensure service SLAs are realistic.
Paper promises without capacity are risky.
SLAs show vendor seriousness.
They separate partners from sellers.
Some SLAs mention response but not resolution.
This creates false comfort.
Hospitals should insist on both.
Response without fix is not enough.
Clear escalation paths should exist.
This prevents endless waiting.
Remote support can solve many issues quickly.
On-site service is still essential for some cases.
Procurement should understand the service mix.
Coverage geography matters.
Vendors should explain how they support remote areas.
Silence here is a risk.
Prosthetics need parts over time.
Batteries, sensors, and joints may fail.
Hospitals should ask about parts availability period.
Support should extend for years, not months.
Lifecycle clarity protects patients.
It also protects hospital reputation.
Technology evolves quickly.
Old models may be discontinued.
Procurement should ask how vendors handle this.
Upgrade paths matter.
A clear obsolescence policy shows maturity.
It prevents stranded users.
Imported parts increase downtime.
Customs delays add uncertainty.
Vendors with local stocking respond faster.
This matters in emergencies.
Hospitals should factor this into evaluation.
Speed saves dignity.
A prosthesis is only as good as its training.
Poor training leads to abandonment.
Hospitals should ensure training is included.
It should not be optional.
Training scope and duration should be defined.
Vagueness leads to shortcuts.
Users change jobs and lifestyles.
Training needs evolve.
Procurement should check if refresher support exists.
This improves long-term outcomes.
Vendors who invest in training reduce failures.
It is a strong quality signal.
Clinicians and therapists need familiarity too.
This supports better follow-up.
Vendor-led staff training builds capability.
It strengthens partnership.
Hospitals should value this support.
It multiplies impact.
When issues arise, documents tell the story.
Missing records create risk.
Hospitals should demand clear documentation.
Device IDs, service logs, and warranty records matter.
Traceability is a safety net.
It supports audits and investigations.
Each prosthesis should be identifiable.
Serial numbers and batch details help.
Hospitals should integrate this into records.
This avoids confusion later.
Good vendors make this easy.
Poor ones resist.
Every service action should be logged.
This builds a history.
Hospitals should have access to these logs.
Transparency builds trust.
Logs also improve care quality.
Patterns emerge over time.
Many hospitals still evaluate prosthetic vendors using simple price tables.
While price matters, this method ignores the long-term cost of failures, rework, and patient dissatisfaction.
A stronger framework looks at total ownership cost.
This includes service load, replacement rates, training effort, and complaint handling.
Descriptive evaluation allows hospitals to defend decisions later.
It shows that value, not just price, drove selection.
Not all prosthetic components carry the same risk.
A failure in a powered hand or knee has higher impact than a cosmetic cover.
Procurement frameworks should assign higher weight to high-risk items.
This ensures quality and service depth are prioritized where consequences are serious.
Hospitals that apply risk-based weighting reduce adverse events.
They also reduce escalation to leadership.
Clinician input is essential but must be structured.
Unstructured opinions can introduce bias.
Hospitals should ask clinicians to score defined parameters.
Comfort, reliability, and ease of service are valid inputs.
This keeps evaluation balanced.
It respects expertise without personal preference dominating.
Hospitals often invite bids before verifying capability.
This leads to wasted time and weak options.
Pre-qualification should confirm certifications, service presence, and product maturity.
Only capable vendors should reach the price stage.
This saves effort later.
It also improves tender quality.
Strong pre-qualification protects procurement credibility.
It shows seriousness.
Certificates, test reports, and service commitments must be verified.
Photocopies and self-declarations are not enough.
Hospitals should insist on verifiable documents.
Online checks are quick and effective.
Verification reduces legal exposure.
It also discourages misrepresentation.
When possible, hospitals should visit vendor facilities.
Seeing manufacturing or service centers reveals much.
Cleanliness, process flow, and staff competence are visible signs.
They cannot be faked easily.
Site visits build confidence.
They also strengthen future collaboration.

Full upfront payment increases risk.
Hospitals lose leverage once payment is released.
Commercial terms should align payment with milestones.
Delivery, fitting stability, and early usage are reasonable points.
This encourages vendor follow-through.
It also aligns with patient outcomes.
Milestones should be realistic.
Fairness sustains partnerships.
Penalties should exist but be proportionate.
They should address repeated or serious failures.
Hospitals must avoid vague penalty language.
Clarity prevents disputes.
Penalties are not about punishment.
They are about accountability.
When defined well, they are rarely used.
Their presence drives discipline.
No partnership lasts forever.
Contracts should define how issues escalate.
Clear escalation paths avoid emotional conflict.
They keep resolution professional.
Termination clauses protect hospitals if risks persist.
They should be fair and structured.
Knowing there is an exit builds confidence.
It enables commitment.
Relying on a single vendor increases vulnerability.
Service disruptions or quality issues can halt care.
Some hospitals approve two vendors per category.
This balances continuity with competition.
Dual sourcing reduces dependency risk.
It also improves negotiation strength.
However, volume should not be spread too thin.
Balance is key.
Before large purchases, hospitals may run pilots.
Limited deployment reveals real-world issues.
Pilots test service SLAs under pressure.
They expose training and support gaps.
This reduces surprises during scale-up.
Learning happens early.
Pilots protect patients and budgets.
They are worth the time.
Procurement should not end at contract signing.
Performance must be reviewed regularly.
Service logs, complaints, and outcomes provide insight.
Trends matter more than single incidents.
Regular reviews encourage improvement.
They keep vendors engaged.
This approach turns procurement into governance.
It elevates its role.
Hospitals pursuing NABH accreditation face strict audit scrutiny.
Prosthetic procurement decisions are reviewed during audits.
Clear documentation, traceability, and vendor control help.
They show system maturity.
Procurement checklists should align with NABH standards.
This reduces audit stress.
Preparation avoids last-minute fixes.
It builds confidence.
When adverse events occur, procurement records are examined.
Incomplete due diligence increases liability.
Hospitals must be able to show why a vendor was chosen.
Evidence of evaluation protects decision-makers.
Clear contracts and records support incident response.
They reduce blame and confusion.
Preparedness is protection.
It matters deeply.
Hospitals are judged by outcomes, not tenders.
Poor prosthetic experiences harm reputation.
Strong procurement prevents these issues quietly.
It is invisible when done right.
Patients remember reliability.
Trust builds through consistency.
Procurement shapes this silently.
Its impact is profound.
At RoboBionics, compliance is not an afterthought.
Our products and processes are designed to meet hospital expectations.
Quality systems, documentation, and traceability are integral.
This supports procurement and audits.
We believe compliance enables innovation.
It does not restrict it.
Hospitals value predictability.
We deliver that.
We understand that service defines prosthetic success.
Our service SLAs are designed around patient urgency.
Local support, remote triage, and rapid resolution are prioritized.
Downtime is treated seriously.
This approach reduces hospital burden.
It improves user trust.
Partnership, not transactions, guide us.
That is our commitment.
We engage procurement teams openly.
Questions are welcomed, not avoided.
Documentation, site visits, and data sharing are part of our process.
Transparency builds confidence.
We see procurement as a clinical ally.
Not a hurdle.
This alignment improves outcomes for all.
Patients benefit most.

Hospitals are moving away from lowest-cost thinking.
Value and accountability are gaining importance.
Prosthetic procurement is at the center of this shift.
Outcomes are visible and personal.
Hospitals that adapt early lead the market.
They attract trust.
Procurement teams become strategic.
Their role expands.
Future procurement will link outcomes with vendor evaluation.
Service quality and patient usage will matter more.
Hospitals should begin collecting basic outcome data now.
This prepares them for future models.
Procurement and clinical teams must collaborate.
Silos weaken systems.
Integration strengthens decisions.
It improves care.
The future belongs to stable ecosystems, not rotating vendors.
Trust and performance compound over time.
Hospitals should invest in relationships that deliver.
Short-term savings rarely last.
A strong ecosystem reduces risk.
It improves resilience.
Procurement leadership defines this future.
Its choices matter.
Every procurement checklist should begin with one clear question: will this prosthesis remain safe and usable for the patient over time.
Price, brand, and delivery speed only matter after this question is answered with confidence.
Hospitals should ensure that safety thinking runs through every checkpoint.
From certification to service response, each item must support long-term use.
This mindset changes how checklists are applied.
They become tools for protection, not paperwork.
Hospitals should first confirm that the vendor operates under a valid quality management system relevant to medical devices.
ISO 13485 certification, with a clear scope that includes prosthetics, should be treated as essential, not optional.
Certification validity must be verified and current.
Expired or unclear certificates should pause procurement, not be explained away.
For powered or advanced prosthetics, testing credibility must be reviewed.
Hospitals should know where testing is done and whether NABL-accredited labs are involved.
These checks create a compliance baseline.
Without them, all other evaluation loses strength.
A prosthesis should not be treated as experimental equipment.
Hospitals should ask how long the product has been in regular clinical use.
Field usage data, even in simple form, adds confidence.
It shows how the device behaves outside brochures.
Hospitals should prefer products already proven in Indian conditions.
Climate, dust, and daily wear patterns matter deeply.
Maturity reduces risk.
It protects both patients and institutions.
Warranty terms must be read as operational documents, not marketing promises.
Hospitals should confirm what is covered, what is excluded, and how claims are handled.
Service SLAs should clearly define response time and resolution time.
A quick call-back without a fix is not real support.
Geographic service coverage must be realistic.
Hospitals should understand how remote or semi-urban patients will be supported.
Clear service assurance reduces future conflict.
It builds trust with users.
Procurement should always ask how long spare parts will be available.
Short-term support creates long-term problems.
Hospitals must understand the vendor’s policy on model discontinuation and upgrades.
Patients should not be stranded by product changes.
Local stocking of critical parts is a strong advantage.
It reduces downtime and stress during failures.
Lifecycle clarity is patient protection.
It also shields hospital reputation.
Initial user training must be included and clearly defined.
A prosthesis without proper training is incomplete care.
Hospitals should also check whether refresher training is available.
User needs evolve over time.
Support for hospital clinicians and therapists matters.
Vendor-led training improves follow-up quality.
Training commitments show seriousness.
They reduce abandonment risk.
Each prosthesis should be traceable to the vendor, batch, and service history.
This is essential for audits and incident reviews.
Hospitals should ensure that service actions are logged and accessible.
Transparency protects all parties.
Good documentation simplifies NABH audits and legal reviews.
It reduces stress during scrutiny.
Traceability is not bureaucracy.
It is safety infrastructure.
When vendors give unclear answers about service timelines or escalation, risk is high.
Strong vendors explain service clearly and confidently.
Evasion or overconfidence without detail should be treated cautiously.
Silence often hides weakness.
Hospitals should insist on written clarity.
Verbal assurances fade quickly.
Service gaps surface later.
Early caution prevents crisis.
Large discounts can signal pressure to close sales.
They may also signal compromises elsewhere.
Hospitals should ask what enables the discount.
Quality, service, or support should not be reduced.
Total value matters more than unit price.
Cheap failures are expensive.
Price should be one factor, not the driver.
Balance protects outcomes.
Vendors who avoid site visits or documentation checks raise concern.
Transparency is a sign of maturity.
Hospitals should be wary of excuses.
Serious partners welcome scrutiny.
Openness builds trust early.
Resistance erodes it.
Procurement should not feel rushed.
Time spent here saves years later.

Procurement choices signal what the hospital values.
Staff notice which vendors are approved and why.
When quality and service are prioritized, care culture strengthens.
Shortcuts become less acceptable.
This influence is subtle but strong.
It shapes behavior over time.
Procurement is leadership.
Its impact extends beyond contracts.
Clinicians perform better when tools are reliable.
Frequent prosthetic issues drain morale.
Strong procurement reduces daily friction.
It allows clinicians to focus on care.
This support is often invisible but deeply felt.
It improves retention and satisfaction.
Reliable systems build confidence.
Confidence improves outcomes.
Patients remember prosthetic success or failure vividly.
Hospitals are judged by these experiences.
Strong procurement prevents negative stories.
It builds positive word-of-mouth slowly.
Reputation grows through consistency.
Procurement decisions enable this.
Quiet success is the goal.
It is achieved through discipline.
At RoboBionics, we work closely with hospital procurement and clinical teams to align with these expectations.
Our approach is built around compliance, transparency, and long-term support.
We invest in quality systems, local manufacturing, and service infrastructure because we know hospitals depend on reliability.
Our documentation, training support, and service SLAs are designed to reduce hospital burden.
We engage procurement teams openly, welcome audits, and believe that clear answers build lasting trust.
Our focus is not just delivery, but sustained patient use and confidence.
For us, procurement success is measured by outcomes, not invoices.
That belief guides how we partner with hospitals across India.
Prosthetic procurement is not a routine purchase.
It is a long-term commitment to patient mobility, dignity, and safety.
Strong checklists protect hospitals legally, clinically, and reputationally.
They turn procurement from a risk point into a strength.
Hospitals that invest time in thoughtful procurement face fewer crises later.
They gain predictability, trust, and respect.
In an era of rising scrutiny and patient awareness, this discipline matters more than ever.
Procurement decisions today shape patient lives tomorrow.
Choosing well is not about complexity.
It is about asking the right questions and insisting on clear answers.
Many hospitals treat procurement checklists as one-time gatekeepers.
Once a vendor is approved, the checklist is forgotten.
In prosthetics, this approach creates blind spots.
Products, people, and service capacity change over time.
Hospitals should convert the checklist into a living system.
Regular reviews keep standards active.
Annual or biannual reassessment is enough.
Consistency matters more than frequency.
Procurement teams rarely hear day-to-day clinical pain points.
This gap weakens decision-making.
Simple feedback loops can fix this.
Quarterly inputs from prosthetists, therapists, and rehab teams add real value.
Patterns of repair, delay, or dissatisfaction should inform vendor scores.
This keeps procurement grounded in reality.
When clinical voices are heard, trust improves.
Systems become smarter, not heavier.
Over time, hospitals build powerful internal data.
Service delays, part failures, and training gaps tell clear stories.
Procurement teams should capture and review these signals.
They predict future problems early.
This turns procurement into risk prevention.
It reduces reactive decision-making.
Data-driven governance builds confidence at leadership level.
It strengthens institutional resilience.
Audits are stressful only when preparation is weak.
Strong procurement systems make audits routine.
Clear vendor files, updated certificates, and service records should be easily accessible.
No scrambling should be required.
Hospitals that maintain audit-ready procurement sleep better.
They respond calmly under scrutiny.
Audit readiness is not extra work.
It is organized work.
When prosthetic issues escalate, procurement decisions come under review.
Hospitals must be able to explain why a vendor was chosen.
A well-documented checklist answers this clearly.
It shows due diligence and reasonable care.
This protects the hospital and its staff.
It also supports fair resolution.
Preparedness reduces blame.
It encourages constructive action.
In legal reviews, intent and process matter.
Hospitals must show that choices were informed and responsible.
Procurement checklists provide this evidence.
They show that decisions followed defined criteria.
This reduces personal risk for committees.
It protects institutional reputation.
Structure is a shield.
It matters more than opinions.
Prosthetics combine medical risk, long-term service, and patient behavior.
This makes them different from most medical purchases.
Procurement teams need basic prosthetic literacy.
Understanding lifecycle, wear, and follow-up changes evaluation quality.
Even short orientation sessions help.
They build confidence and accuracy.
Knowledge reduces dependency on vendor claims.
It empowers teams.
Strong hospitals do not isolate procurement.
They involve clinical, rehab, and quality teams.
Cross-functional committees reduce blind spots.
They balance cost, care, and compliance.
These committees do not need to meet often.
Even periodic reviews add value.
Shared ownership improves decisions.
It also spreads accountability.
Procurement decisions affect real lives.
Teams should be reminded of this.
Ethical framing improves judgment.
It shifts focus from speed to safety.
Hospitals that reinforce patient-first procurement build strong culture.
Culture outlasts policies.
This mindset protects everyone.
It defines institutional character.

Patients today ask more questions.
They research devices and expect explanations.
Hospitals will face greater scrutiny on choices.
Procurement transparency will matter.
Strong systems prepare hospitals for this future.
Weak ones will struggle.
Accountability is rising.
Preparation is the only answer.
Procurement will increasingly link with outcomes.
Service quality and patient use will influence vendor standing.
Hospitals should begin aligning procurement with outcome thinking.
This transition takes time.
Early movers gain confidence and control.
Late movers face pressure.
Value-based care is coming.
Procurement must be ready.
The future favors stable partnerships.
Constant vendor rotation increases risk.
Hospitals that build trusted ecosystems gain predictability.
Quality improves steadily.
Procurement leaders shape this future.
Their choices compound over years.
Stability benefits patients most.
That is the true goal.
Hospital prosthetic procurement is not a routine operational task.
It is a long-term promise to patients who depend on mobility for dignity and livelihood.
A strong procurement checklist built around ISO, NABL awareness, warranty depth, and service SLAs protects that promise.
It safeguards hospitals clinically, legally, and reputationally.
When procurement is done with care and clarity, problems reduce quietly.
Clinicians feel supported, patients feel secure, and leadership feels confident.
At RoboBionics, we believe hospitals deserve partners who respect this responsibility.
We design our systems, services, and documentation to support safe, transparent procurement.
Choosing the right prosthetic partner is not about complexity.
It is about asking clear questions and expecting clear answers.
That discipline is what turns procurement into a pillar of patient trust.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.