Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
Many prosthetic delays do not happen because of surgical problems or device limitations. They happen

Doctors are often asked to justify why a certain prosthetic choice makes sense, not just clinically but financially. Hospitals, insurers, and even families want proof that outcomes are worth the cost. Randomized trials rarely reflect daily practice, especially in prosthetic care. This is where real-world evidence becomes powerful. Simple, consistent documentation from routine clinical work can strongly support cost-effectiveness claims. This article explains, in very clear terms, what real-world evidence means, why it matters so much today, and how clinicians can document care in a way that naturally builds strong, defensible evidence over time.
Real-world evidence is simply information collected while doing normal clinical work.
It does not require special studies, extra forms, or research grants.
Every fitting, follow-up, repair, and rehab session already generates data.
When this information is recorded with intention, it becomes evidence.
In prosthetic care, this kind of evidence is often more trusted than trials.
It reflects real patients, real settings, and real constraints.
Decision-makers increasingly value this realism.
It answers practical questions, not theoretical ones.
Clinical trials usually exclude complex cases.
They follow strict protocols that rarely match daily practice.
Prosthetic outcomes depend on behavior, environment, and service quality.
These factors are hard to control in trials.
Real-world evidence captures these messy realities.
It shows what actually happens after the device leaves the clinic.
For cost-effectiveness, this matters deeply.
Costs and benefits emerge over time, not just at delivery.
Every time a clinician notes progress, comfort, usage, or problems,
they are creating a data point.
When multiple patients show similar patterns,
those notes become a trend.
Trends are the backbone of real-world evidence.
They explain why certain choices work better.
The only missing step is consistency.
Structured notes turn scattered facts into proof.
Many clinicians know their patients do well.
They see fewer breakdowns and better adherence.
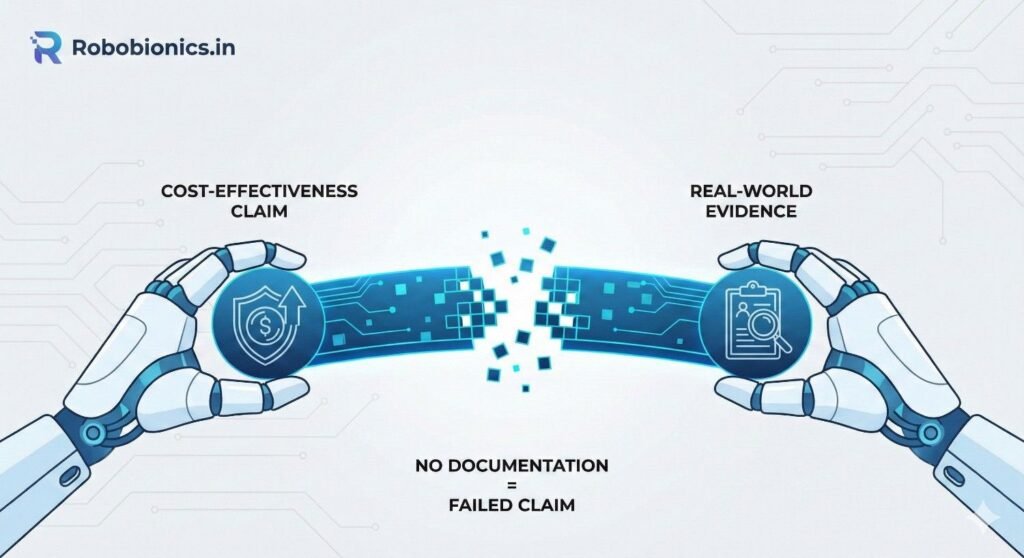
But without documentation, these observations remain anecdotal.
Anecdotes are weak in financial discussions.
Hospitals and insurers ask for patterns, not opinions.
They need evidence that can be reviewed later.
Without records, even excellent care appears unproven.
This is a missed opportunity.
System-level decisions are made far from the clinic.
Committees rarely meet patients.
They rely on files, summaries, and numbers.
If those are incomplete, decisions suffer.
Clinicians may lose access to preferred devices or approaches,
not because they are ineffective,
but because effectiveness was never documented clearly.
Documentation bridges this gap.
It carries the clinician’s voice forward.
When outcomes are unclear, costs feel higher.
Decision-makers assume inefficiency.
A device that performs well but lacks follow-up notes
may appear risky or expensive.
Clear documentation shows how costs are offset by outcomes.
Fewer visits, fewer repairs, and higher use matter.
Without this context, cost-effectiveness claims collapse.
The value story remains untold.
Simple measures of function matter.
Walking distance, grip confidence, task completion.
These do not need complex tools.
Consistent observation is enough.
Recording how function changes across visits
shows whether progress is steady or stalled.
Steady progress supports cost-effectiveness.
It shows value unfolding over time.
A prosthesis that is not used has zero value.
Usage is a core outcome.
Clinicians often ask about daily use.
Writing this down consistently is key.
Notes like “used daily for work”
carry more weight than vague satisfaction scores.
Over time, usage patterns tell a powerful story.
They explain why some devices deliver better value.
Cost-effectiveness is strongly influenced by service load.
Repairs, adjustments, and emergency visits add cost.
Clinicians already know which patients need frequent help.
Recording frequency and reasons makes this visible.
When certain choices reduce service burden,
documentation proves it.
This evidence speaks directly to payers and hospitals.
It links outcomes to cost control.
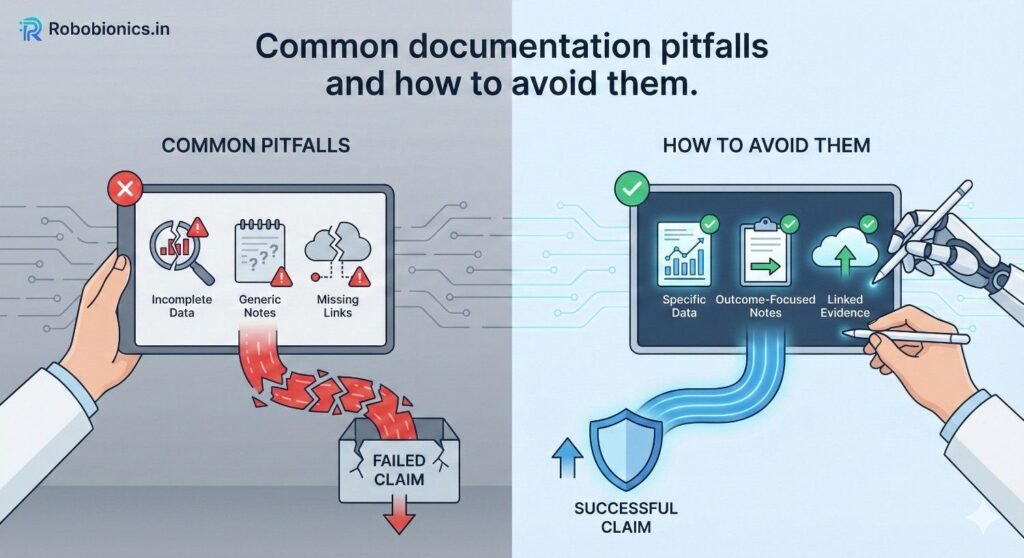
Clinical notes are often written only for immediate care.
But many others may read them later.
Writing clearly helps non-clinical reviewers understand value.
Simple language works best.
Avoiding shorthand and unexplained abbreviations helps.
Clarity improves credibility.
Each note becomes part of a larger narrative.
That narrative supports cost-effectiveness claims.
Consistency allows comparison.
If every clinician writes differently, patterns hide.
Using similar phrases for comfort, usage, and issues
makes trends easier to spot.
This does not require rigid templates.
It requires shared habits.
Over time, consistency turns notes into datasets.
Datasets carry influence.
Clinicians often document problems more than success.
This skews perception.
Recording absence of issues is equally important.
“No breakdowns since last visit” matters.
Negatives show stability.
Stability is a cost-effectiveness driver.
Balanced documentation reflects reality better.
It strengthens evidence.

Follow-ups often focus on immediate complaints.
They should also capture outcomes.
A simple note on comfort, confidence, and daily use
adds long-term value.
These notes take little time.
They add significant evidence.
Over multiple visits,
they show trajectories rather than snapshots.
Trajectories are persuasive.
They explain why early choices matter.
Patients describe their lives in simple terms.
Clinicians should record those words.
Statements like “I can work full day now”
are powerful evidence.
They link clinical care to life impact.
Life impact drives cost-effectiveness.
Avoid over-medicalizing patient voices.
Plain language carries authenticity.
Rehab intensity affects results.
Documenting effort provides context.
When progress is good,
notes show why.
When progress is slow,
notes explain contributing factors.
This context protects clinicians.
It also improves interpretation of outcomes.
Documentation should not feel like extra work.
It should fit naturally.
Most clinics already use SOAP-style notes.
Adding a few outcome-focused lines is enough.
Small changes repeated often
create large datasets over time.
This approach respects clinician time.
It builds evidence quietly.
Asking the same few questions at each visit
standardizes data.
Questions about daily use, comfort, and confidence
are simple and fast.
Writing brief answers captures value.
No scales or scores needed.
Consistency beats complexity.
It makes evidence usable.
Electronic records can support structure.
But they should not overwhelm.
Simple dropdowns or prompts help.
Too many fields discourage completion.
Clinicians should help design practical templates.
Usability matters.
Good design increases adoption.
Adoption builds evidence.
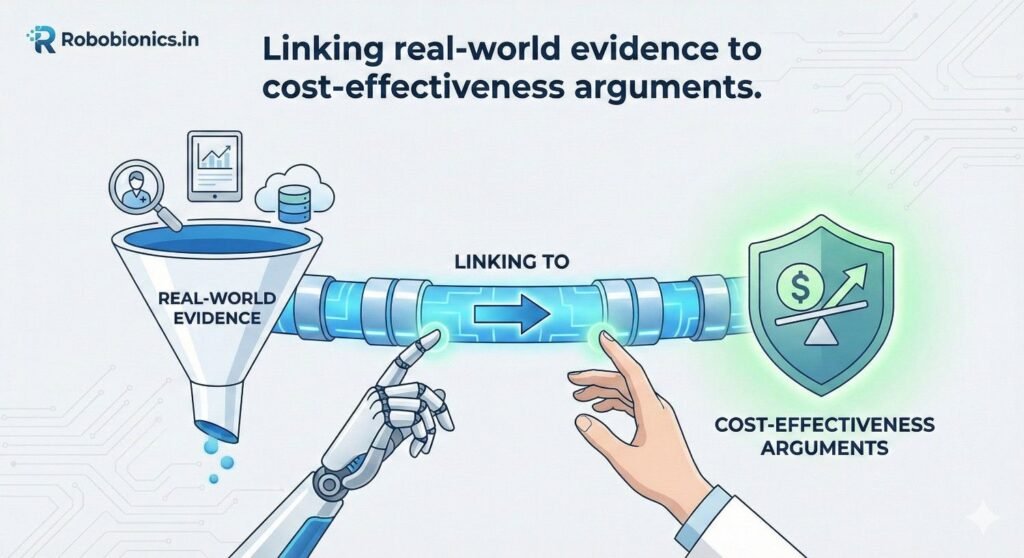
When clinicians talk about cost-effectiveness, the most common mistake is focusing only on the device price rather than on what happens after delivery. Real-world evidence allows doctors to show how outcomes unfold over months and years, and how these outcomes quietly offset the initial cost through reduced service needs, better function, and sustained use. This is where documentation becomes powerful, because it captures the ongoing story rather than a single transaction.
For example, when notes consistently show stable use, good comfort, and minimal adjustments across follow-ups, they demonstrate that the chosen solution requires less ongoing input. This reduced service burden translates directly into lower long-term cost, even if the upfront price is higher. When clinicians can point to their own patient records to show this pattern, cost-effectiveness arguments move from theory to lived proof.
Hospitals and payers often default to comparing prices because outcomes feel harder to measure. Clinician documentation can gently shift this conversation by making outcomes visible and concrete. When records clearly show faster functional gains, fewer complications, and sustained independence, the focus naturally moves toward value delivered rather than money spent.
Doctors do not need to calculate cost per outcome themselves. They need to document outcomes in a way that allows others to see the link. When documentation shows that patients require fewer visits, fewer repairs, and less intensive rehab, decision-makers can easily connect these dots. The clinician’s role is to ensure those dots exist in the first place.
Single visits rarely prove anything. Cost-effectiveness emerges across time. Real-world evidence is strongest when it shows consistent patterns across many patients and many months. This is why follow-up documentation matters more than initial fitting notes.
When clinicians record steady progress, stable use, and low complication rates across their patient population, they create a longitudinal picture of value. This picture is far more persuasive than isolated success stories. Over time, such patterns form the backbone of strong internal reports, reimbursement discussions, and even policy submissions.
Reimbursement discussions often stall because medical necessity appears limited to the moment of fitting. Real-world evidence extends necessity across the care journey by showing how continued use supports function, safety, and independence. Clinician notes that describe how a prosthesis enables work, mobility, or daily living tasks make necessity ongoing rather than episodic.
When documentation shows that removing or downgrading a device would reduce function or increase dependency, it strengthens reimbursement arguments. These records show that the prosthesis is not optional or cosmetic, but central to the patient’s health and participation. This framing resonates strongly with payers reviewing long-term claims.
Upgrades and advanced components often face scrutiny because their value is questioned. Real-world evidence allows clinicians to justify these choices based on observed outcomes rather than promises. When notes show limitations with basic solutions and measurable improvements after changes, the upgrade becomes defensible.
Clear documentation of problems before the upgrade, followed by improvements in comfort, use, or function after, creates a before-and-after narrative. This narrative is far more convincing than abstract claims. It shows that cost increases were tied to real need and real benefit.
Many reimbursement denials stem from unclear or incomplete reasoning rather than from disagreement about outcomes. Clinician documentation that explains why a particular approach was chosen, based on patient needs and context, reduces ambiguity.
When reasoning is explicit and linked to observed outcomes, reviewers have less room to question intent. Clear notes protect both the patient and the clinician by showing that decisions were thoughtful, patient-centered, and evidence-informed.
Hospital committees often include non-clinical members who rely heavily on written records. Clinician documentation becomes their primary window into patient outcomes. Notes that clearly describe functional gains, stability, and reduced complications help committees understand why certain approaches should be supported.
When clinicians document in plain language that links care decisions to patient outcomes, they make it easier for committees to approve protocols and partnerships. This clarity reduces friction and speeds decision-making.
Hospitals are cautious about changing standard practices. Real-world evidence from within the institution carries special weight because it reflects local conditions, patient populations, and workflows. When clinicians document consistent success with certain approaches, they provide internal proof that change is safe and beneficial.
Over time, this internal evidence can support updates to care pathways and procurement policies. Clinicians who document well contribute not only to individual patient care, but also to system-level improvement.
Clear documentation also protects clinicians during audits or quality reviews. When outcomes and reasoning are well recorded, decisions are easier to defend. This protection reduces stress and builds confidence in practice.
Auditors are not looking for perfection. They are looking for consistency and logic. Real-world evidence, when documented clearly, meets this need effectively.
Clinicians often assume that data analysis requires specialized software or research teams. In reality, many insights can be drawn from simple aggregation of routine notes. Even basic counts of follow-up visits, repairs, or reported use can reveal meaningful patterns.
When documentation uses consistent language and categories, simple reviews become possible. This allows clinics to summarize outcomes periodically without heavy effort. These summaries strengthen cost-effectiveness discussions at multiple levels.
Clinicians do not need to analyze data alone. Administrators, quality teams, and prosthetic partners often have the capacity to support aggregation and presentation. Good documentation makes collaboration easier because the raw material is already there.
When clinicians and partners work together, real-world evidence can be transformed into reports, presentations, and policy inputs. This collaboration amplifies the impact of everyday documentation.
While building evidence, clinicians must always respect privacy and consent norms. Aggregation should focus on patterns, not on exposing individual identities. Ethical handling of data preserves trust and credibility.
When evidence is built responsibly, it strengthens the profession rather than risking harm. Ethical practice and strong evidence go hand in hand.

The biggest barrier to better documentation is the belief that it adds work. In reality, it is a shift in focus rather than an increase in time. Writing notes with outcomes in mind changes emphasis, not length.
Clinicians who understand how their notes influence larger decisions are more motivated to document clearly. Purpose transforms routine tasks into meaningful contributions.
Documentation improves fastest when teams agree on shared habits. Peer discussions about what to note and how to phrase observations create alignment. This alignment improves data quality across the clinic.
Shared standards do not need to be rigid. They need to be practical and agreed upon. This balance supports adoption without resistance.
Clinicians should receive feedback on how their documentation is used. When doctors see their notes supporting approvals or reimbursement, the value becomes tangible. This feedback loop reinforces good habits.
Over time, documentation quality improves naturally when its impact is visible. Evidence-building becomes part of professional identity rather than an administrative burden.
Clinicians often see documentation as a record of care, but in today’s systems it also functions as a bridge between clinical reality and financial decision-making. Every note connects what happened in the clinic to how that care will later be judged by hospitals, payers, and policymakers. When documentation reflects outcomes clearly and consistently, it allows value to travel beyond the consultation room.
This mindset shift is essential. Instead of asking what must be written to close a file, clinicians can ask what future reader might need to understand why this care made sense. This does not require longer notes. It requires clearer intent. Over time, this clarity builds a body of real-world evidence that supports cost-effectiveness naturally, without special effort.
Across all prosthetic cases, three outcome anchors matter most for cost-effectiveness: function, use, and stability. Function reflects what the patient can do. Use reflects whether the prosthesis is actually part of daily life. Stability reflects how often problems interrupt that life. When clinicians document these three anchors consistently, the value story becomes clear.
Function shows benefit. Use shows relevance. Stability shows sustainability. Together, they explain why costs are justified and why certain choices reduce long-term burden. Even brief notes that touch on these anchors, visit after visit, accumulate into strong evidence. This approach keeps documentation focused and meaningful rather than scattered.
Cost-effectiveness is rarely proven in a single moment. It emerges across months and years. Clinicians do not need to prove everything at once. They need to let time work in their favor by recording outcomes consistently.
When records show that patients remain active, require fewer interventions, and maintain use over time, the cost argument strengthens automatically. Delays, setbacks, and challenges can also be documented honestly. What matters is the trajectory. Longitudinal patterns are more persuasive than perfect snapshots.
When asked whether a prosthetic choice is worth the cost, clinicians can point to real-world outcomes rather than abstract claims. They can explain that patients with similar profiles have shown sustained use, fewer service needs, and better function over time, as reflected in routine follow-up records.
This response feels grounded and credible because it is based on lived experience rather than marketing or isolated studies. It reassures decision-makers that value has been observed repeatedly, not promised hypothetically. Documentation makes this confidence possible.
Newer solutions often face skepticism because their long-term value is uncertain. Real-world evidence reduces this uncertainty by showing early patterns of benefit and stability. Clinicians can document how patients adapt, how often adjustments are needed, and how use evolves over time.
When early real-world outcomes are visible and transparent, skepticism softens. Decision-makers understand that evidence is being built responsibly rather than assumed. This openness strengthens trust and supports responsible innovation.
Patients sometimes ask clinicians to support appeals or approvals. Clear documentation allows clinicians to advocate effectively without emotional appeals alone. When records show consistent benefit and necessity, advocacy becomes factual rather than persuasive.
This protects clinicians from appearing biased and protects patients from arbitrary decisions. Evidence-based advocacy is calmer, stronger, and more successful.
Many records focus heavily on problems, while periods of stability go undocumented. This creates a distorted picture where care appears reactive and inefficient. Clinicians should document stability and success with the same care as complications.
Notes that say a patient is doing well, using the device daily, and not needing adjustments are powerful. They show that the system is working. Over time, these quiet successes define cost-effectiveness more than rare crises.
Phrases like “patient satisfied” or “doing okay” lack meaning for reviewers. They do not explain what is working or why. Slightly more descriptive language adds clarity without adding length.
Describing specific activities, comfort levels, or changes in routine makes outcomes tangible. This specificity improves the usefulness of documentation for anyone evaluating value later.
Some clinicians avoid any language that could be interpreted as financial. While clinicians should not discuss costs directly in notes, documenting outcomes that influence cost is appropriate and important.
Reduced visits, fewer repairs, and stable use are clinical facts with financial implications. Recording them does not compromise ethics. It supports transparency and responsible care.
Strong real-world evidence emerges when entire teams document with similar intent. Prosthetists, therapists, and clinicians should align on what outcomes matter and how they are described. This alignment reduces variation and strengthens patterns.
Leadership can support this by encouraging discussion and sharing examples of effective notes. When teams see how documentation supports approvals or reduces disputes, motivation increases naturally.
Periodic reviews of aggregated outcomes help teams see the impact of their work. These reviews do not need to be formal research meetings. Even simple discussions about trends in use, repairs, or progress reinforce learning.
When clinicians see patterns across patients, their confidence in certain approaches grows. This confidence feeds back into better care and clearer documentation.
Prosthetic providers and technology partners play an important role in supporting evidence-building. Partners who encourage outcome tracking, provide follow-up support, and respect documentation needs strengthen the entire ecosystem.
Clinicians should seek partnerships that align with evidence-based practice rather than those focused only on transactions. Alignment here improves both outcomes and credibility.

Real-world evidence is not about turning clinicians into researchers. It is about recognizing that everyday care already generates powerful proof when it is documented thoughtfully. In prosthetic care, where outcomes depend on long-term use, behavior, and service quality, this kind of evidence is especially valuable.
Cost-effectiveness claims become stronger when they are rooted in routine clinical reality rather than abstract models. Clear documentation allows clinicians to show how value unfolds over time, how costs are offset by stability and function, and why certain choices make sense beyond price tags.
At RoboBionics, we believe that clinicians are the most credible source of real-world evidence. When their voices are captured clearly through documentation, the system listens. Better decisions follow, not because costs are ignored, but because value is finally visible.
Thoughtful documentation is not an administrative task. It is an extension of care. It ensures that good outcomes are not just achieved, but also recognized, protected, and sustained for the patients who depend on them.
Many prosthetic delays do not happen because of surgical problems or device limitations. They happen
Traumatic amputations place doctors under intense pressure to save life first, but the decisions made
Amputation after cancer is not just a surgical event. It is the end of one
When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.