
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
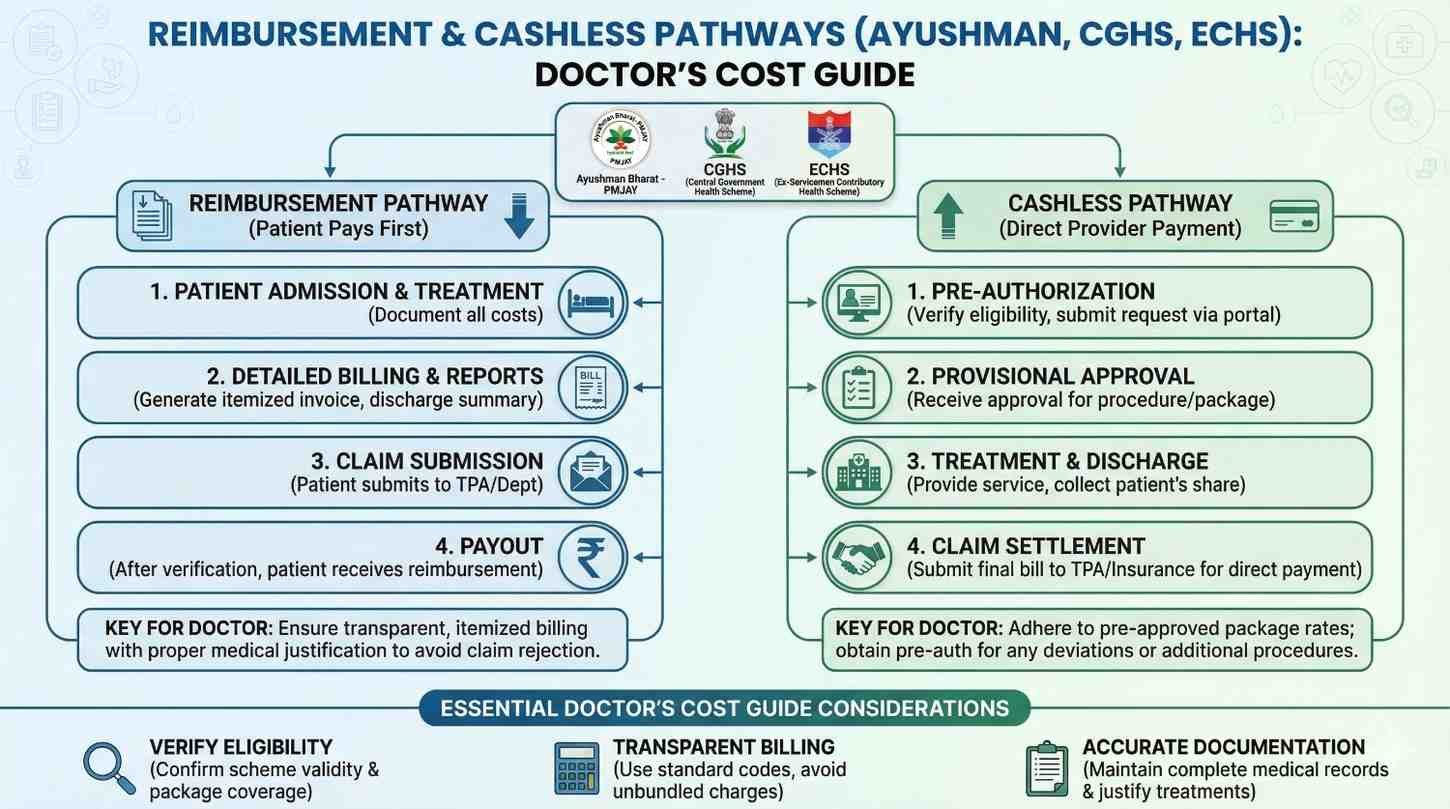
For a doctor in India, prescribing a prosthetic is never just a medical decision. It is also a money decision. The right limb can change a life, but only if the patient can actually pay for it or get it approved. This is where many good prescriptions fail. Files move slowly, rules are unclear, and patients feel lost.
This guide is written to make that path clear. In simple words, it explains how reimbursement and cashless schemes work for prosthetic care under Ayushman Bharat, CGHS, and ECHS. It is focused on cost, approvals, documents, and common problems doctors face every day. The aim is to help you guide patients with confidence, reduce delays, and improve success rates from prescription to delivery.
Many patients receive the right medical advice but never receive the device.
This gap is rarely clinical. It is financial and procedural.
Patients often return after weeks saying the scheme rejected the file.
At that point, trust breaks and outcomes suffer.
For most patients, the doctor is the only trusted guide.
They do not understand schemes, packages, or rates.
A few clear words from the doctor can save months of confusion.
This guidance often decides whether care moves forward or stops.
Delayed prosthetics lead to muscle loss and poor training.
Pain, falls, and skin issues increase with time.
Early approval and delivery improve long-term success.
Reimbursement clarity directly affects medical results.
Clear files reduce back-and-forth with TPAs and scheme officers.
This saves time for doctors and hospital staff.
Fewer rejections mean fewer angry follow-ups.
Systems run smoother when the first submission is correct.

Ayushman, CGHS, and ECHS cover a large patient base.
They are the most common routes for prosthetic funding.
Each scheme has its own logic and limits.
Mixing them up leads to rejection.
Ayushman works mainly on cashless hospital claims.
CGHS and ECHS are mostly reimbursement-driven.
This single difference changes how doctors should advise patients.
It affects timelines, documents, and vendor choice.
Schemes only pay through approved hospitals.
Some also require approved prosthetic vendors.
If either is missing, payment stops.
Doctors must check this early, not after prescription.
Ayushman treats prosthetics as part of a treatment package.
It is not always a separate line item.
The logic is hospital-led, not device-led.
This is important while writing notes.
Ayushman uses fixed package rates.
These rates may not match modern prosthetic costs.
Doctors should align expectations early.
Overpromising creates distress later.
If the hospital is empanelled, care can be cashless.
Pre-authorization is mandatory in most cases.
Clinical notes must clearly justify functional need.
Vague words often lead to queries.
Files fail due to missing diagnosis clarity.
Laterality and amputation level are often unclear.
Another issue is mismatch between package and device.
This can be reduced with correct coding.
CGHS patients usually pay first.
They claim reimbursement later.
This affects how cost is discussed.
Transparency is critical from day one.
CGHS has defined rate lists.
Prosthetics often fall under capped categories.
If costs exceed limits, patient pays the difference.
Doctors should explain this clearly.
CGHS relies heavily on written justification.
Functional need must be explained simply.
Words like daily activity, safety, and independence help.
Short notes often lead to partial payment.
Reimbursement is not instant.
It can take weeks or months.
Patients should be prepared mentally and financially.
This avoids panic calls later.
ECHS serves ex-servicemen and dependents.
They often expect structured processes.
However, prosthetics still need careful handling.
Rules vary by region and polyclinic.
ECHS requires referral from a polyclinic.
Direct private treatment may not be accepted.
Doctors must check referral letters carefully.
Missing stamps cause delays.
ECHS follows its own approved rates.
Only certain vendors may be accepted.
Early vendor confirmation saves time.
Late changes almost always fail.
ECHS may ask for higher-level approval.
This increases processing time.
Doctors should flag this early.
Patients appreciate honest timelines.
Simple, functional language works best.
Avoid technical jargon without explanation.
Focus on what the patient cannot do.
Then explain how the prosthesis helps.
Schemes pay for function, not features.
Doctors should connect limb loss to daily tasks.
Walking, eating, working, and safety matter.
This framing improves acceptance.
Missing limb side is a frequent error.
So is unclear amputation level.
Dates, signatures, and stamps must be clear.
Small errors cause big delays.
Doctors should explain scheme limits upfront.
This avoids shock later.
Even one clear sentence helps.
Silence often leads to false hope.
Some patients qualify for multiple schemes.
The cheapest path is not always the fastest.
Doctors can help weigh time versus money.
This guidance builds trust.
Not all advanced devices are fully covered.
Patients should know this early.
Framing it as an upgrade helps.
Surprises damage relationships.
Vendors understand scheme paperwork deeply.
Early coordination reduces rejection risk.
Doctors should loop them in early.
This is not a conflict, it is teamwork.
A short call saves many emails.
Explain why a device is chosen.
This helps vendors prepare correct quotes.
Alignment improves speed.
Changing device specs late is risky.
Schemes may reject revised files.
Doctors should finalize intent before submission.
Stability matters more than perfection.
For most schemes, the prosthetic is never seen as a single product.
It is viewed as part of an entire treatment journey, which includes surgery history, rehabilitation, follow-up, and long-term use.
Doctors often quote or think only of the device cost.
However, schemes look at total episode cost, and this mismatch causes confusion and rejection.
Understanding this difference helps doctors frame recommendations better.
It also prepares patients for what is covered and what may not be.
Direct costs include the prosthetic limb, socket, and basic fitting.
These are usually the only parts considered by reimbursement bodies.
Indirect costs like training, follow-ups, travel, and adjustments are often ignored.
Patients end up paying these silently.
Doctors who explain this early help patients plan better.
This honesty strengthens long-term trust.
Most schemes treat prosthetics as a one-time expense.
They do not fully account for wear, tear, or upgrades.
In reality, users need replacements and changes over time.
Doctors should gently explain this long-term reality.
This helps families avoid emotional shock later.
It also allows realistic life planning.
Ayushman packages are reviewed by non-clinical teams.
They rely heavily on written notes and coding accuracy.
If the medical need is not obvious on paper, it is questioned.
Even valid cases can get stuck.
Doctors must assume the reviewer has no prosthetic knowledge.
Clear explanations matter more than advanced terms.
In many cases, prosthetics are expected to be part of surgical care.
Standalone prosthetic claims are harder to pass.
If amputation was recent, linking it to surgery helps.
If old, justification must be stronger.
Doctors should mention rehabilitation necessity clearly.
This shows continuity of care.
Ayushman patients often expect full coverage.
This belief comes from how the scheme is advertised.
Doctors must gently explain package limits.
This conversation is uncomfortable but necessary.
When handled early, patients accept reality better.
When delayed, anger is directed at doctors.

CGHS rates are conservative and slow to change.
They often lag behind modern prosthetic technology.
Doctors should know the current ceiling rates.
This helps guide realistic prescriptions.
Recommending a device far above limits needs explanation.
Otherwise, patients feel misled.
CGHS still values physical documents strongly.
Illegible writing is a common rejection cause.
Doctors should ensure notes are readable and complete.
A clear stamp and signature matter more than we think.
These small steps save months of delay.
They also reduce follow-up queries.
CGHS patients often worry after paying upfront.
The waiting period creates anxiety.
Doctors can reduce stress by explaining timelines.
Even rough timeframes help patients stay calm.
A short reassurance during follow-up visits goes a long way.
It shows care beyond prescription.
ECHS rules are interpreted differently across locations.
What works in one city may fail in another.
Doctors should avoid assumptions.
Local verification is always safer.
Speaking to the polyclinic early saves time.
It also prevents patient frustration.
ECHS paperwork must match exactly.
Dates, ranks, and referral numbers must align.
Even small mismatches trigger rejection.
Doctors should double-check referral letters.
Encouraging patients to keep copies helps.
Lost documents cause long delays.
ECHS patients often expect fast resolution.
They are used to structured systems.
Doctors should explain civilian vendor involvement carefully.
This avoids confusion and mistrust.
Clear communication builds cooperation.
It makes the process smoother for everyone.
Many patients qualify for a scheme but use the wrong route.
They may approach a non-empanelled hospital or vendor.
Doctors who identify this early save the case.
Late correction is often impossible.
Asking one extra question during consultation helps.
It can change the entire outcome.
Some files fail despite eligibility.
The reason is often weak medical explanation.
Doctors may assume limb loss is self-explanatory.
Reviewers do not see it that way.
Explaining function loss improves approval chances.
This is a small but powerful change.
Patients may want high-end prosthetics.
Schemes may only support basic versions.
Doctors must balance hope with honesty.
Clear upgrade discussions are essential.
When done well, patients respect transparency.
Surprises create anger.

At the first visit, ask about scheme eligibility.
This should be routine, not awkward.
Understanding coverage early shapes recommendations.
It also avoids wasted effort.
Doctors should note scheme details in records.
This helps future coordination.
Confirm hospital and vendor empanelment.
This step is often skipped.
A quick check saves weeks later.
It also protects the patient.
Doctors should align internally with admin teams.
Teamwork reduces errors.
Write in simple, functional language.
Avoid assumptions.
Mention diagnosis, level, side, and daily impact.
Clarity improves success.
Encourage patients to submit files promptly.
Delays increase rejection risk.
Doctors are trained to focus on care, not cost.
Discussing money can feel wrong.
However, ignoring cost harms patients more.
It leads to broken care journeys.
Learning to speak calmly about money helps.
It is part of modern medical care.
Cost talks should feel supportive.
They are about planning, not refusal.
Using words like options and pathways helps.
It keeps hope alive.
Patients value honesty over silence.
Trust grows through clarity.
In reimbursement-driven prosthetic care, the file matters as much as the limb.
Many rejections happen not because the care is unnecessary, but because the story is incomplete on paper.
Approving officers do not see the patient, the gait, or the struggle.
They only see what is written, and they decide based on that alone.
Doctors who understand this reality write differently.
They document with the reviewer in mind, not just the medical record.
Across Ayushman, CGHS, and ECHS, certain documents are repeatedly asked for even if not clearly listed.
These include a clear diagnosis note, amputation level, laterality, date of event, and a functional recommendation.
When any one of these is unclear, queries begin.
Each query adds weeks to the process.
Doctors can reduce this by being slightly more detailed upfront.
One extra sentence can prevent months of delay.
Schemes respond better to function than to features.
A note that says “myoelectric hand required” is weaker than one that explains why.
Explaining that the patient needs to eat independently, return to work, or avoid falls makes the need real.
This framing aligns with how schemes justify public spending.
Doctors should connect the device to daily life.
This improves approval odds across all pathways.
Patients often ask, “How long will this take?”
The honest answer depends on the scheme, location, and file quality.
Ayushman approvals may come in days if clean.
CGHS and ECHS reimbursements often take weeks or months.
Doctors should avoid exact promises.
Instead, they should explain ranges and reasons.
When patients expect fast payment and it does not happen, anxiety rises.
They begin calling doctors, hospitals, and vendors repeatedly.
This stress damages trust even if the doctor did nothing wrong.
Clear expectation-setting prevents this cycle.
A calm explanation early saves emotional energy later.
Patients feel guided, not abandoned.
During follow-ups, doctors can briefly ask about the claim status.
This shows care beyond the prescription.
Even saying “these things take time” reassures patients.
Silence often feels like neglect.
Small check-ins improve the overall experience.
They cost nothing but build confidence.

Many doctors see rejection as final.
In reality, many cases succeed on appeal.
Rejections often highlight what is missing.
They are feedback, not judgement.
Doctors who read rejection notes carefully can fix gaps.
This approach saves many cases.
Adding clearer functional justification is the most effective fix.
Clarifying limb level or diagnosis also helps.
In some cases, attaching rehab notes strengthens the file.
This shows continuity of care.
Appeals should be calm and factual.
Emotional language rarely helps.
Doctors do not need to chase offices.
Their main role is improving the medical note.
A revised note with clearer language often unlocks stalled files.
This is where medical authority matters most.
Doctors should support patients during this phase.
Guidance here is deeply appreciated.
Manufacturers understand scheme rules in detail.
They see patterns across hundreds of cases.
Doctors who coordinate early avoid wrong quotes and wrong codes.
This alignment reduces rejection risk.
This is not commercial influence.
It is operational efficiency.
Instead of naming a device first, doctors should share goals.
Grip strength needs, work tasks, or terrain challenges matter more.
Manufacturers can then suggest scheme-aligned options.
This keeps costs within limits where possible.
Early discussion avoids last-minute changes.
Late changes often break approvals.
Patients benefit from faster approvals and fewer surprises.
They also feel supported by a team, not individuals.
This teamwork reduces emotional load.
Care feels smoother and more humane.
Not every patient needs the most advanced option.
Function, environment, and goals should guide choice.
Schemes usually support basic functional needs.
Upgrades can be discussed transparently.
Doctors should help patients match need to option.
This reduces financial regret.
Repeated hospital visits increase travel and wage loss.
Clear planning reduces unnecessary trips.
Tele-consult reviews and bundled visits help.
Doctors can suggest these when appropriate.
Lower indirect cost improves adherence.
Patients stay engaged longer.
A prosthetic journey lasts years, not weeks.
Doctors should think beyond first delivery.
Explaining maintenance and future needs helps families plan.
This prevents shock later.
Long-term clarity builds resilience.
It improves overall outcomes.
Doctors walk a fine line.
Too much optimism creates false hope.
Too much caution feels like denial.
Balance comes from facts and empathy.
Clear explanation with options works best.
Patients respect honesty.
Cost discussions should never feel judgmental.
They should feel practical and supportive.
Using calm, neutral language helps.
Tone matters as much as content.
Patients remember how they were spoken to.
This shapes trust deeply.
Doctors are anchors in uncertain systems.
Their words carry weight.
Even when systems fail, guidance matters.
Patients feel less alone.
This human role cannot be replaced.
It is central to good care.
Reimbursement pathways are complex, but they are navigable.
When doctors understand cost logic, schemes, and documentation, outcomes improve.
Patients receive devices sooner.
Stress reduces across families and clinics.
This knowledge is now part of clinical responsibility.
Ignoring it harms care more than addressing it.
At RoboBionics, we work daily within these systems.
We support doctors with clarity, documentation help, and realistic cost planning.
When medical intent and financial pathways align, prosthetic care succeeds.
That alignment is where lives truly change.

In India, the same scheme behaves differently across states and cities.
This is not written in any rulebook, but every experienced doctor has seen it happen.
Local officers interpret guidelines based on past cases and local pressures.
What is accepted easily in one region may face questions in another.
Doctors should never assume uniformity.
Local awareness is a quiet advantage.
Ayushman Bharat is centrally designed but state-run.
Each state adds its own processes, portals, and checkpoints.
Some states approve prosthetic-linked packages quickly.
Others are cautious and seek repeated clarification.
Doctors practicing near state borders often notice this contrast sharply.
Knowing your state’s behavior helps in planning and counseling.
CGHS reimbursement offices vary in workload and speed.
Metro cities often face backlog, while smaller cities may process faster.
Some offices insist on strict adherence to rate lists.
Others allow partial flexibility with strong justification.
Doctors who learn their local office style save patients time.
This knowledge usually comes from repeated exposure.
ECHS is structured, but not identical everywhere.
Different commands and polyclinics interpret rules differently.
Some insist on strict vendor lists.
Others focus more on referral correctness.
Doctors should advise patients to follow local polyclinic guidance closely.
Ignoring this often leads to rejection.
Under Ayushman, basic prosthetic support may be included within a package.
However, advanced devices are rarely fully covered.
If a device cost exceeds the package value, the gap becomes self-pay.
Doctors should explain this gently.
Using realistic examples during counseling helps patients decide calmly.
Abstract numbers confuse people.
CGHS often reimburses up to a fixed ceiling.
Anything above that is patient responsibility.
Doctors should know approximate ceilings for common prosthetics.
This avoids uncomfortable surprises later.
When recommending beyond ceilings, justification must be strong.
Even then, partial reimbursement is common.
ECHS rates are often closer to CGHS than market prices.
This creates a gap for modern devices.
Doctors should explain this gap early.
Patients appreciate honesty.
In some cases, ECHS may approve higher costs after review.
But timelines increase significantly.
Many patients learn about advanced prosthetics online.
They come with high expectations.
Schemes, however, focus on basic function.
This creates tension.
Doctors should frame upgrades as optional improvements.
Not as medical necessities unless truly justified.
Patients should never feel pushed.
They should feel informed.
Explaining what the scheme covers first creates a baseline.
Upgrades can then be discussed calmly.
This approach respects patient autonomy.
It also protects the doctor ethically.
When patients choose self-pay upgrades, documentation matters.
Written consent protects everyone.
Doctors should ensure patients understand cost differences.
This avoids disputes later.
Transparency builds trust.
Silence breaks it.

Always ask about insurance or scheme eligibility.
This should become routine.
Note the scheme clearly in records.
This helps all future steps.
Set early expectations about timelines and limits.
This reduces stress later.
Confirm hospital and vendor empanelment.
This single step saves weeks.
Align internally with admin teams.
Coordination prevents errors.
Decide the prosthetic intent clearly.
Avoid late changes.
Use simple, functional language.
Assume a non-medical reviewer.
Mention diagnosis, level, side, and daily impact.
Clarity matters more than length.
Avoid vague terms.
Specifics improve approval chances.
Encourage patients to track their files.
Passive waiting often delays things.
Offer reassurance during follow-ups.
Even brief check-ins help.
Be open to revising notes if needed.
Appeals often succeed with clarity.
Reimbursement systems are complex, but they are not impossible.
They reward clarity, patience, and planning.
Doctors who understand cost pathways improve outcomes without compromising care.
Patients reach mobility sooner and with less distress.
This knowledge is now part of modern clinical responsibility.
Ignoring it leaves patients unsupported.
At RoboBionics, we work alongside doctors every day.
We help align medical intent with real-world pathways.
When clinical care and financial access move together, prosthetic success becomes predictable.
That is how independence is restored, not just prescribed.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.