
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
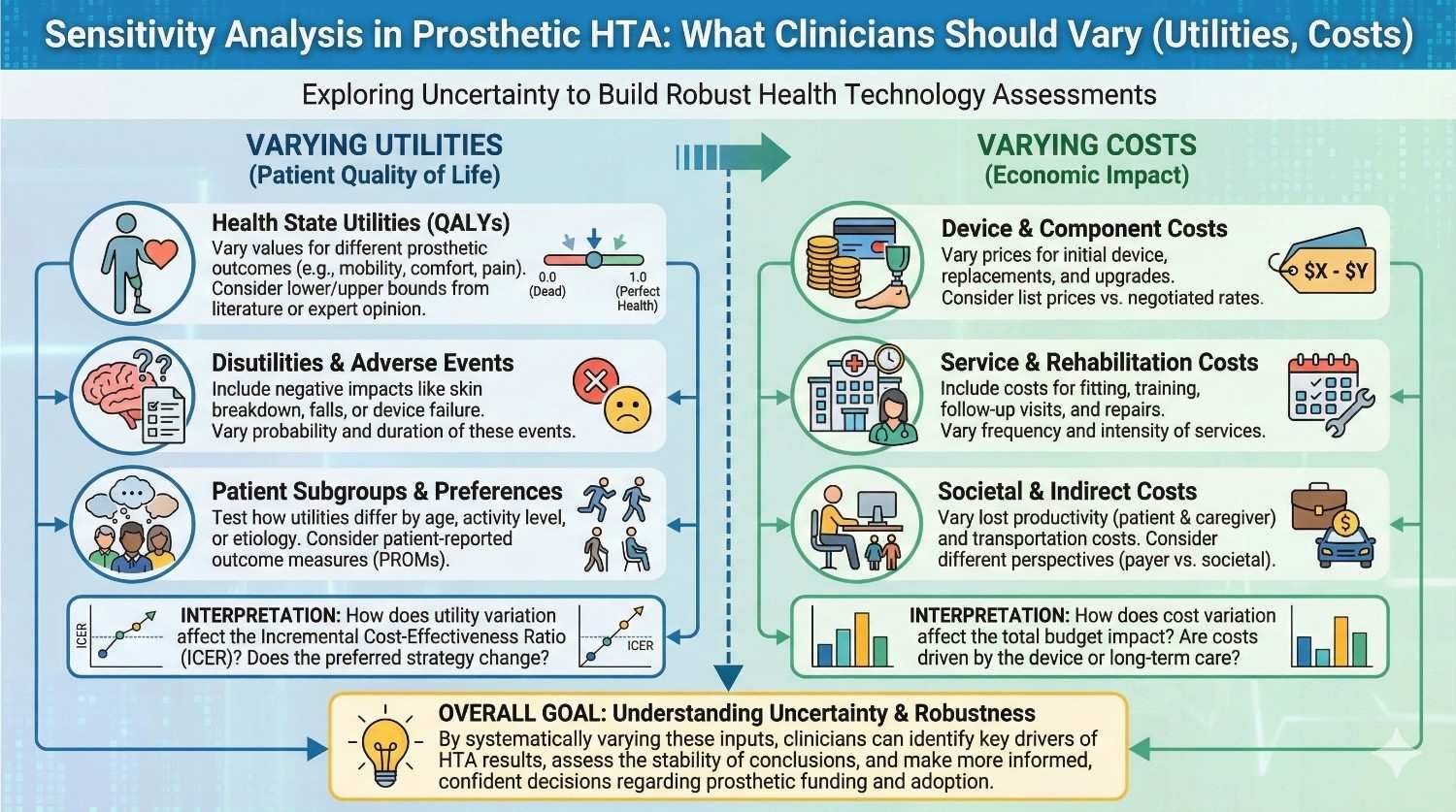
Health Technology Assessment sounds complex, but the core idea is simple. It asks one honest question: if numbers change a little, does the decision still make sense? In prosthetic care, this question matters deeply. Costs vary, patient lives differ, and outcomes are never identical. Sensitivity analysis helps clinicians test their assumptions before systems, payers, or patients test them the hard way.
This article is written for clinicians who want clarity, not theory. It explains what sensitivity analysis means in prosthetic HTA, which numbers actually matter, and how to vary them in a practical, Indian context. The goal is not to turn doctors into economists, but to help them defend good clinical decisions with calm confidence and simple logic.
In prosthetic care, no two patients live the same life, even when the diagnosis looks identical on paper.
Daily activity, family support, work demands, and local terrain change how much benefit a prosthesis truly delivers.
Sensitivity analysis accepts this reality instead of ignoring it.
It asks whether a decision still holds when real life pushes the numbers up or down.
Doctors are increasingly asked to justify choices to hospitals, insurers, and government schemes.
A single-point estimate often looks weak when questioned.
Sensitivity analysis gives clinicians a range, not a guess.
This makes discussions calmer and decisions easier to defend.
Some prosthetic choices only make sense if everything goes perfectly.
If one assumption fails, the whole plan collapses.
Sensitivity analysis exposes these weak points early.
It helps clinicians avoid decisions that break under pressure.
Sensitivity analysis asks what happens when one input changes.
The outcome is observed while everything else stays the same.
If the result changes a lot, that input is important.
If the result barely moves, that input is less critical.
In prosthetic HTA, inputs include cost, comfort, usage time, and quality of life.
Outcomes usually relate to value, cost-effectiveness, or long-term benefit.
Sensitivity analysis shows which assumptions truly drive value.
This clarity helps clinicians focus on what matters most.
Even if doctors never build a full model, they influence the inputs.
Their notes define utilities, timelines, and expected outcomes.
Understanding sensitivity helps clinicians write better justifications.
It also helps them question unrealistic expectations early.
Utility is a number that tries to reflect quality of life.
In prosthetics, it represents comfort, independence, safety, and dignity.
It is not just about walking or gripping.
It includes confidence, social participation, and reduced fear.
A prosthesis may change one person’s life completely and another’s only slightly.
Age, job type, and family support shape this difference.
Sensitivity analysis allows this spread to be tested.
It avoids assuming the same benefit for every user.
Utilities often come from questionnaires or past studies.
Clinician interpretation affects how these are applied.
By understanding sensitivity, doctors can argue for realistic ranges.
This makes assessments fairer and closer to real life.

Many models assume a fixed number of daily usage hours.
In reality, usage changes with comfort, weather, and work demands.
Varying usage time shows how fragile value claims can be.
Clinicians should test both optimistic and conservative scenarios.
Some prosthetics can do many things but are used for few.
The gap between ability and actual use is important.
Sensitivity analysis should reduce assumed gains gradually.
This reflects real adoption patterns more honestly.
Confidence and social ease are hard to measure.
They are often overestimated without intent.
Varying these values tests whether conclusions rely too much on emotion.
Balanced models respect both physical and mental benefit.
The device price is only one part of the journey.
Training, repairs, and follow-up add significantly over time.
Sensitivity analysis should stretch these costs upward.
This prepares models for real-world expense.
Many models assume ideal maintenance cycles.
Actual wear depends on use intensity and environment.
Varying replacement timelines shows long-term cost risk.
This is critical in Indian conditions.
Travel, lost wages, and caregiver time are rarely fixed.
They change across regions and families.
Including ranges for these costs improves realism.
It also aligns models with patient experience.
One-way sensitivity analysis changes a single variable.
Everything else remains constant.
This shows which factor influences results most strongly.
It is simple and easy to explain.
Clinicians often debate one issue at a time.
Cost, comfort, or durability usually lead the conversation.
One-way analysis mirrors this thinking style.
It supports clear, focused discussions.
Changing values unrealistically creates misleading results.
Ranges should reflect real clinical variation.
Clinicians can help set sensible bounds.
Their experience keeps analysis grounded.
In real life, variables rarely change alone.
Higher usage may increase both benefit and maintenance cost.
Multi-way analysis reflects this linked movement.
It gives a more honest picture of uncertainty.
Advanced prosthetics often involve trade-offs.
Higher function may bring higher training needs.
Multi-way analysis shows whether value survives complexity.
This protects against overly optimistic conclusions.
Doctors understand how variables interact clinically.
They know which changes tend to occur together.
Their insight improves scenario design.
This makes assessments more credible.
Threshold analysis asks how far a value can fall before a decision changes.
It identifies the tipping point.
This is powerful in payer discussions.
It shows limits clearly.
A clinician can say a device remains valuable even with lower usage.
This strengthens the case for approval.
Thresholds turn debate into numbers.
They reduce emotional back-and-forth.
Clear limits feel honest.
They show the doctor has considered uncertainty.
This transparency builds confidence with patients and payers.
It reflects responsible decision-making.

Published studies often report neat averages.
Real patients rarely behave like averages.
Sensitivity analysis should question these values.
Clinicians should push for wider ranges.
Some users stop using prosthetics early.
Models often assume continuous use.
Varying dropout rates is essential.
It prevents inflated benefit claims.
Training outcomes depend on motivation and support.
Assuming perfect training success is risky.
Sensitivity analysis should lower success rates.
This tests robustness honestly.
Understanding sensitive variables helps clinicians write better notes.
They can emphasize factors that truly drive value.
This improves approval success.
It aligns clinical language with HTA logic.
Patients ask whether a prosthesis is worth it.
Sensitivity thinking allows honest answers.
Doctors can explain best and worst cases calmly.
This supports informed consent.
Sensitivity analysis discourages extreme promises.
It encourages balanced guidance.
Clinicians who think this way protect patients.
They also protect their own credibility.
Sensitivity analysis becomes meaningful only when it begins with a real decision a clinician faces.
For example, whether to recommend a basic mechanical hand or a myoelectric hand for a working adult is not a theoretical problem, but a daily one.
The clinical intent may be clear, but the financial and outcome uncertainty is not.
Sensitivity analysis helps test whether the recommendation holds when assumptions change.
This approach keeps the analysis grounded in patient care.
It prevents numbers from drifting away from clinical reality.
Every analysis starts with a base case.
This is the most likely scenario based on clinical judgement.
In prosthetic care, the base case might assume regular daily use, stable health, and standard follow-up.
It should not assume perfect behavior or ideal conditions.
Clinicians are best placed to define this middle path.
Their experience gives the base case credibility.
Not all outcomes deserve equal attention.
Walking stability, ability to work, and safety often matter more than abstract scores.
Sensitivity analysis should focus on outcomes that change lives.
Clinicians should guide analysts toward these endpoints.
This keeps the assessment patient-centered.
It also makes results easier to explain.
A prosthesis used by a daily wage worker faces harsher conditions than one used in an office job.
Usage intensity, fatigue, and wear differ significantly.
Sensitivity analysis should lower utility for high-strain contexts.
It should raise it modestly for supportive environments.
This variation reflects lived reality.
It avoids one-size-fits-all conclusions.
Younger users may adapt faster and use devices longer each day.
Older users may value safety and comfort more than speed.
Utilities should be varied across age groups.
This helps test whether value claims hold across life stages.
Clinicians understand these patterns well.
Their input makes models more humane.
Initial excitement often fades.
Long-term satisfaction depends on comfort and reliability.
Sensitivity analysis should reduce utility after the first year in some scenarios.
This tests durability of benefit.
Such adjustments prevent overly optimistic lifetime projections.
They align models with long-term follow-up data.

In Indian settings, dust, heat, and moisture increase wear.
Maintenance costs are rarely as low as brochures suggest.
Sensitivity analysis should raise maintenance costs gradually.
Clinicians can suggest realistic ranges.
This prepares decision-makers for real expenses.
It avoids later disappointment.
Some users outgrow sockets or change body weight quickly.
Replacement may be needed earlier than planned.
Varying replacement intervals reveals long-term cost risk.
This is especially important for young users.
Clinicians see these patterns firsthand.
Their insight is critical here.
Patients traveling long distances face higher indirect costs.
Missed work and fatigue add hidden burdens.
Sensitivity analysis should expand these costs in rural scenarios.
This improves equity in assessments.
Models that ignore this often undervalue care.
Clinicians can correct this bias.
Scenario analysis groups multiple changes together.
This reflects real-world complexity better than single changes.
A best-case scenario assumes good adherence and low complications.
A difficult-case assumes interruptions and higher support needs.
Clinicians intuitively think this way.
Formalizing it strengthens arguments.
When presenting to boards or payers, scenarios clarify uncertainty.
They show preparedness, not doubt.
Clinicians can explain why a decision survives even in harder cases.
This builds confidence.
Scenarios reduce confrontational debates.
They shift focus to resilience of care plans.
Scenarios should stay plausible.
Extreme assumptions weaken credibility.
Clinicians should challenge unrealistic analyst inputs.
Their role is to keep scenarios believable.
Balanced scenarios are persuasive.
They reflect responsible care planning.
Threshold analysis helps answer how much improvement is enough.
For example, how much daily use justifies a higher-cost prosthesis.
Clinicians often know this intuitively.
Formal thresholds help communicate it.
This clarity supports difficult conversations.
It aligns expectations.
If value collapses below a certain usage level, clinicians can plan safeguards.
Extra training or follow-up can be built in.
Thresholds guide supportive interventions.
They make care proactive.
This approach improves outcomes.
It also protects investments.
Patients appreciate honesty about limits.
Explaining that benefit depends on use encourages engagement.
This is not discouraging.
It is empowering.
Patients feel part of the decision.
Trust deepens.
Sensitivity analysis discourages absolute statements.
It replaces them with ranges and possibilities.
This tone feels respectful to patients.
It acknowledges uncertainty without fear.
Patients respond better to honesty.
It builds long-term cooperation.
Every prosthetic choice involves trade-offs.
Cost, comfort, and capability must be balanced.
Sensitivity analysis frames these trade-offs visually and verbally.
It helps patients choose consciously.
Clinicians become guides, not persuaders.
This strengthens ethics.
When patients understand best and worst cases, regret reduces.
Outcomes feel expected, not disappointing.
Sensitivity analysis supports this clarity.
It protects emotional well-being.
This is an often overlooked benefit.
But it is powerful.

Many clinicians worry sensitivity analysis is too technical.
In reality, it starts with simple questions.
You do not need software to think in ranges.
You need clinical honesty.
Small steps are enough.
They make a big difference.
Time is limited.
Sensitivity thinking can be brief.
Even asking what happens if use is lower helps.
This mindset fits into routine care.
It improves decisions without slowing clinics.
Efficiency remains intact.
Some fear that admitting uncertainty weakens authority.
In practice, it strengthens credibility.
Balanced explanations build respect.
Patients and payers trust thoughtful clinicians.
Sensitivity analysis is not hesitation.
It is responsibility.
Sensitivity analysis should not sit with one person.
Teams should share this mindset.
Clinicians, therapists, and coordinators can all contribute.
Each sees different variables.
This collective view improves assessments.
It creates shared ownership.
Real-world outcomes should inform future ranges.
Follow-up teaches what assumptions were right or wrong.
Clinicians should feed this back into thinking.
This closes the learning loop.
Over time, decisions become sharper.
Uncertainty reduces.
Sensitivity analysis must reflect Indian conditions.
Climate, access, and social support matter.
Clinicians are the best translators of these realities.
Their voice is essential.
This ensures HTA serves people, not just numbers.
That is its true purpose.
When clinicians think in terms of ranges rather than fixed promises, their documentation becomes more honest and more defensible.
Instead of writing that a prosthesis will restore full function, notes can reflect expected benefit under normal use while acknowledging that outcomes depend on training, comfort, and regular wear.
This approach does not weaken the prescription.
It shows that the clinician has considered real-world variability and has planned care responsibly.
Such notes align well with HTA logic and payer review.
They demonstrate foresight rather than doubt.
Utility does not need to be written as a number in the medical record.
It can be expressed through expected changes in daily life, independence, safety, and ability to work.
By describing best-case and typical outcomes in words, clinicians indirectly reflect a sensitivity range.
Reviewers understand that benefit is not binary.
This narrative style feels natural in clinical practice.
It bridges medicine and evaluation without added burden.
Clinicians often hesitate to mention cost variability in notes.
However, acknowledging the need for follow-up, maintenance, and possible adjustments shows realism.
Phrases that explain the need for ongoing support help justify long-term value.
They signal that the prosthesis is part of care, not a one-time object.
This framing supports reimbursement discussions.
It also protects patients from false expectations.

Payers worry about misuse, abandonment, and cost overruns.
Sensitivity-informed notes directly address these fears.
By showing that value remains even with conservative assumptions, clinicians build trust.
They show that the decision is not fragile.
This alignment improves approval rates.
It reduces repeated queries and delays.
When a claim is questioned or rejected, sensitivity thinking provides a strong base for appeal.
Clinicians can explain that even with lower usage or higher cost, the prosthesis remains justified.
This shifts the discussion from absolute cost to value stability.
It reframes the conversation constructively.
Appeals grounded in such reasoning feel professional.
They are harder to dismiss.
Payers are sensitive to over-prescription concerns.
Sensitivity analysis shows restraint and thoughtfulness.
Clinicians who document uncertainty demonstrate ethical care.
They show that patient benefit, not device promotion, drives decisions.
This tone builds institutional credibility.
It supports long-term collaboration.
Sensitivity thinking naturally limits overstatement.
It encourages clinicians to explain ranges and conditions.
Patients are better prepared for variation.
They feel respected rather than sold to.
This honesty reduces disappointment.
It supports emotional well-being.
Hope is essential in prosthetic care.
But hope must survive contact with reality.
Sensitivity analysis helps clinicians offer grounded hope.
It frames improvement as likely, not guaranteed.
Patients appreciate this balance.
It builds durable trust.
When patients understand uncertainty, they make better choices.
They can weigh effort, cost, and benefit consciously.
Sensitivity-informed discussions empower patients.
They turn decisions into partnerships.
This respect strengthens consent.
It aligns with ethical practice.
Younger clinicians often learn fixed answers.
Sensitivity thinking teaches them to ask deeper questions.
Mentoring around ranges and scenarios builds maturity.
It prepares them for real-world complexity.
This mindset improves long-term care quality.
It reduces rigid thinking.
Each follow-up visit provides data.
Clinicians see where assumptions held and where they failed.
Feeding this insight back into future decisions sharpens judgement.
Over time, ranges become more accurate.
This learning loop is powerful.
It turns experience into structured wisdom.
Manufacturers see long-term use patterns.
Clinicians see patient adaptation.
Sharing this knowledge improves sensitivity ranges.
It makes assessments more grounded.
At RoboBionics, we value this exchange deeply.
It improves outcomes for everyone.

Begin every major prosthetic decision with a realistic middle path.
Avoid best-case fantasies or worst-case fear.
This anchors judgement.
It sets a fair starting point.
Ask what happens if one important factor changes.
Usage, comfort, or follow-up adherence are good choices.
If value collapses, the plan needs support.
If it holds, confidence increases.
If benefit depends on training or comfort, strengthen those areas.
Schedule extra follow-ups or rehab.
This proactive step improves outcomes.
It reduces regret.
Write notes that reflect thoughtfulness.
Explain expectations and dependencies briefly.
This protects the patient and the clinician.
It aligns with HTA principles naturally.
Sensitivity analysis is not about numbers alone.
It is about humility, honesty, and preparedness.
In prosthetic care, uncertainty is not a flaw.
It is a reality to be managed.
Clinicians who embrace sensitivity thinking make stronger decisions.
They protect patients from fragile plans and unrealistic promises.
At RoboBionics, we see this every day.
When clinicians think in ranges and plan for variation, outcomes improve.
Prosthetic success is not built on perfect assumptions.
It is built on resilient decisions that hold even when reality shifts.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.