
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
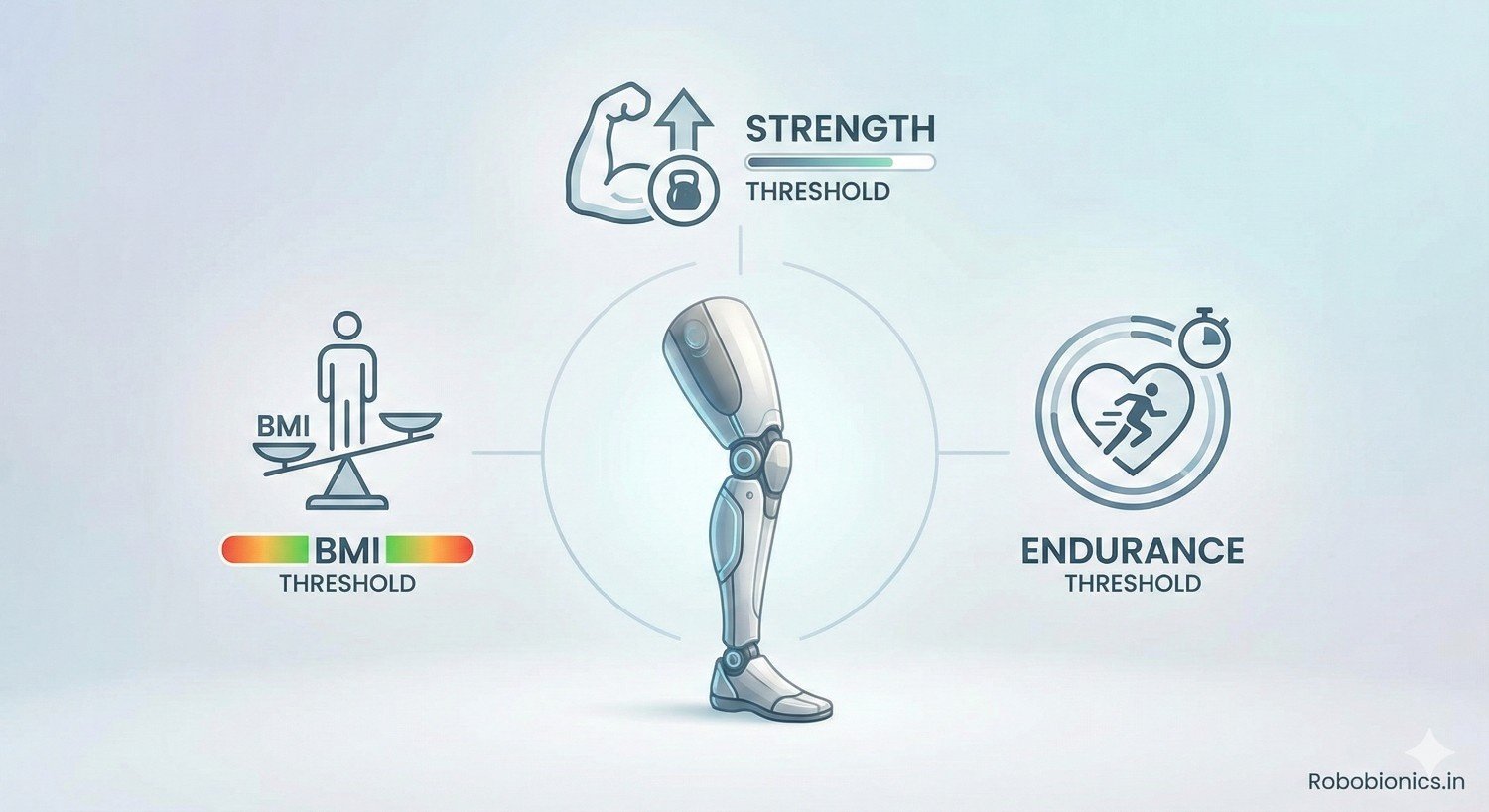
Prosthetic success does not depend on technology alone. It depends on whether the body can safely carry, control, and sustain the effort that a prosthetic demands every day. For doctors and rehabilitation teams, this means looking closely at body weight, muscle strength, and endurance before prescribing a device. These physical factors shape safety, comfort, and long-term use more than many people realize.
At Robobionics, we work with patients across a wide range of body types and fitness levels. We have seen strong outcomes when physical readiness is assessed honestly, and poor outcomes when it is ignored. A prosthetic that is too demanding for the body often leads to pain, falls, and early abandonment. A prosthetic that matches the body’s capacity supports confidence and independence.
This article focuses on BMI, strength, and endurance thresholds for prosthetic candidates. It explains why these factors matter, how doctors can assess them in simple ways, and how thresholds guide safe decision-making. The goal is not to exclude patients, but to prepare them properly and choose solutions that work in real life.
If you are a clinician, therapist, or part of an amputee care team, this guide will help you make clearer, safer choices. When physical readiness is understood and respected, prosthetic care becomes more effective and more humane.
A prosthetic is not just worn, it is actively carried and controlled by the body throughout the day.
Every step, transfer, or reach places extra load on muscles, joints, and the heart.
If the body cannot tolerate this load, even the best prosthetic becomes unsafe.
Doctors often focus on healing and limb shape, but physical capacity determines daily success.
Thresholds help predict whether the body can handle repeated effort without breakdown.
Ignoring these limits increases pain, fatigue, and fall risk.
Patients who meet basic physical thresholds tend to use their prosthetic more consistently.
They recover faster after activity and feel more confident during movement.
This consistency is key for long-term acceptance.
When thresholds are not met, use becomes irregular.
The prosthetic may be worn only briefly or avoided altogether.
Matching capacity to demand protects outcomes.
Physical thresholds are not meant to deny care.
They help doctors plan preparation, timing, and device choice.
Many patients can improve their readiness with guided support.
Using thresholds early allows safer progression.
Patients understand what needs to improve and why.
This transparency builds trust and motivation.
BMI gives a general view of body weight relative to height.
In prosthetic care, it helps estimate load on joints and sockets.
Higher BMI increases mechanical stress during movement.
While BMI is not perfect, it is a useful starting point.
It helps doctors anticipate fitting challenges and endurance demands.
BMI should always be interpreted alongside other factors.
Very low BMI often means low muscle mass and poor cushioning.
These patients may experience pressure pain and skin breakdown.
Socket comfort becomes harder to achieve.
Low body reserve also affects endurance.
Fatigue appears quickly during training.
Strength building may be needed before fitting.
Doctors should assess nutritional status carefully.
Improving weight and muscle supports safer prosthetic use.
Timing matters more than speed.
High BMI increases force through the prosthetic and remaining limb.
This stresses joints, skin, and cardiovascular systems.
Energy cost of walking rises significantly.
Socket suspension may be less stable with higher weight.
Skin folds and sweating increase irritation risk.
Fit must be managed carefully.
High BMI does not exclude prosthetic use.
It requires stronger components and endurance planning.
Weight management improves outcomes over time.
There is no single BMI cutoff for prosthetic eligibility.
However, extremes at either end increase risk.
Context always matters.
Doctors should consider BMI trends, not just numbers.
Recent weight loss or gain affects readiness.
Stability is often more important than absolute value.
BMI should be discussed openly with patients.
Clear explanation reduces stigma.
Shared understanding improves cooperation.
Heavier patients require components rated for higher loads.
This affects durability and safety.
Using under-rated components increases failure risk.
For low BMI patients, softer interfaces may be needed.
Pressure distribution becomes critical.
Component choice must match body composition.
BMI helps guide these technical decisions.
It protects both patient and device.
Thoughtful selection improves longevity.
Certain BMI-related issues suggest waiting before fitting.
Poor wound healing, skin fragility, or extreme fatigue are signs.
These indicate limited tolerance.
Delaying fitting allows targeted preparation.
Nutrition, conditioning, and medical optimization help.
This improves later success.
Explaining the reason for delay is essential.
Patients accept waiting when benefits are clear.
Honesty prevents frustration.
Strength controls balance, posture, and movement efficiency.
A prosthetic amplifies weakness if muscles cannot stabilize it.
Falls often result from strength deficits, not device failure.
Key muscle groups differ by amputation level.
Hips, core, and shoulders often compensate.
Weakness here limits safety.
Doctors should assess functional strength.
Simple movements reveal real capacity.
This guides safe planning.
Lower limb prosthetic use demands strong hips and core.
These muscles control weight shift and stance.
Knee stability depends on them.
Patients must stand, turn, and recover balance.
Without adequate strength, effort skyrockets.
Fatigue leads to unsafe movement.
Strength testing should focus on functional tasks.
Chair rises and step control are informative.
These predict walking safety.
Upper limb prosthetics rely on shoulder and trunk strength.
Lifting, positioning, and control require endurance.
Weak shoulders limit functional reach.
Many patients compensate with the opposite limb.
Overuse injuries may develop.
Balanced strength reduces strain.
Doctors should assess bilateral capacity.
This supports realistic expectations.
Strength guides device complexity.
Rather than isolated muscle grades, doctors should use functional benchmarks.
Tasks like repeated sit-to-stand or supported balance tell more.
These reflect real-life demands.
Patients who struggle with basic tasks may not tolerate prosthetic load.
This signals need for conditioning first.
Preparation reduces risk.
Benchmarks should be explained clearly.
Patients appreciate concrete goals.
This improves engagement.
After amputation, strength often becomes uneven.
One side works harder than the other.
This imbalance affects prosthetic control.
Compensation may hide weakness initially.
Over time, pain and fatigue appear.
Early detection prevents injury.
Doctors should assess both sides carefully.
Symmetry improves efficiency.
Balanced strength supports long-term use.
Sometimes healing is complete but strength is not.
This is a common reason for early failure.
Strength deficits should not be ignored.
Delaying fitting to build strength is protective.
It avoids negative learning and fear.
Patients progress faster later.
Clear explanation is essential.
Patients must understand the benefit.
This builds trust in the process.
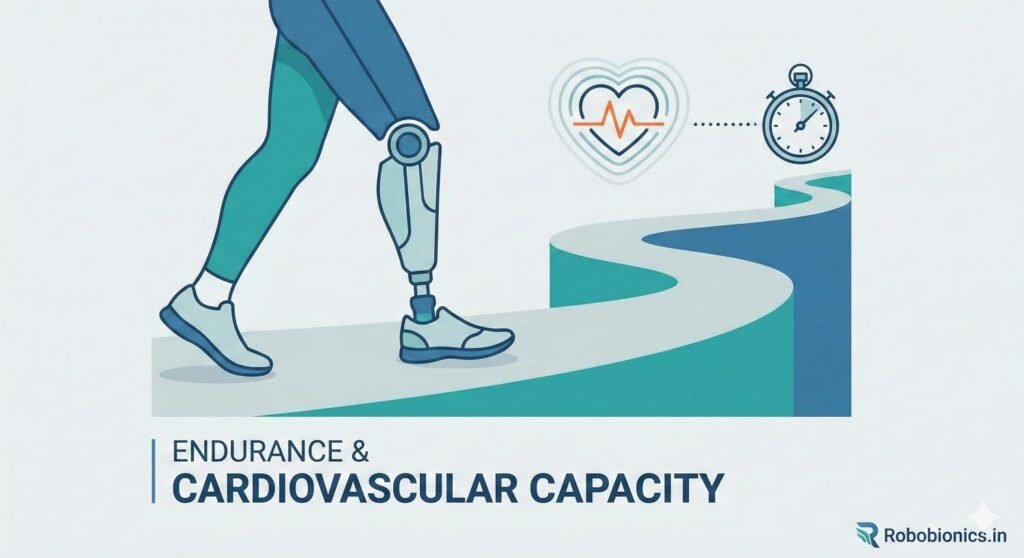
Prosthetic use requires sustained effort, not short bursts.
Walking with a prosthetic increases energy use.
Endurance determines how long activity can be maintained.
Patients with poor endurance tire quickly.
Fatigue affects balance and judgment.
This increases fall risk.
Endurance is often underestimated.
Doctors should assess it intentionally.
It predicts real-world use.
Prosthetic walking demands more from the heart and lungs.
Energy cost rises with amputation level and BMI.
Patients with heart or lung disease are affected more.
Short clinic walks may appear fine.
Longer daily use tells a different story.
Assessment should reflect daily life.
Doctors should consider medical history carefully.
Cardiac clearance may be needed.
Safety must guide decisions.
Many patients start strong and fade quickly.
This reveals limited endurance reserve.
Training must respect this pattern.
Ignoring fatigue leads to setbacks.
Rest becomes part of progress.
Gradual build-up improves tolerance.
Endurance thresholds guide pacing.
They protect long-term success.
Overload harms confidence.
Doctors do not need complex equipment.
Timed walking or standing tasks provide insight.
Recovery time is equally important.
Patients who recover slowly may struggle daily.
This indicates limited reserve.
Endurance building may be needed first.
Assessments should be repeated.
Consistency matters more than peak effort.
Patterns guide planning.
Dizziness, breathlessness, or confusion signal overload.
These should not be ignored.
They indicate unsafe demand.
Doctors must stop training when signs appear.
Pushing through fatigue is dangerous.
Safety outweighs speed.
Clear communication helps patients understand limits.
This prevents guilt or frustration.
Education supports cooperation.
Endurance can often be improved.
Pre-prosthetic conditioning is valuable.
It prepares the body gradually.
Simple activities build tolerance.
Consistency matters more than intensity.
Progress should be monitored.
Improved endurance shortens later rehab.
Patients feel more capable.
Preparation pays off.
BMI, strength, and endurance interact constantly.
A patient may be strong but lack endurance.
Another may have endurance but poor strength.
Decisions must consider all three together.
Focusing on one creates blind spots.
Integrated assessment improves accuracy.
Doctors should view thresholds as a system.
Balance matters more than extremes.
Holistic planning improves safety.
High BMI with low endurance is common.
Low BMI with poor strength also appears often.
Each pattern needs a different approach.
Recognizing these patterns helps tailor preparation.
Generic plans fail.
Specific strategies succeed.
Patients benefit from personalized explanations.
They understand their own profile.
Engagement improves.
Goals must match what the body can sustain.
This may mean limited walking or part-time use.
Realistic goals prevent disappointment.
As capacity improves, goals can expand.
Progress should feel earned.
This builds confidence.
Doctors should revisit goals regularly.
Capacity changes over time.
Flexibility is key.
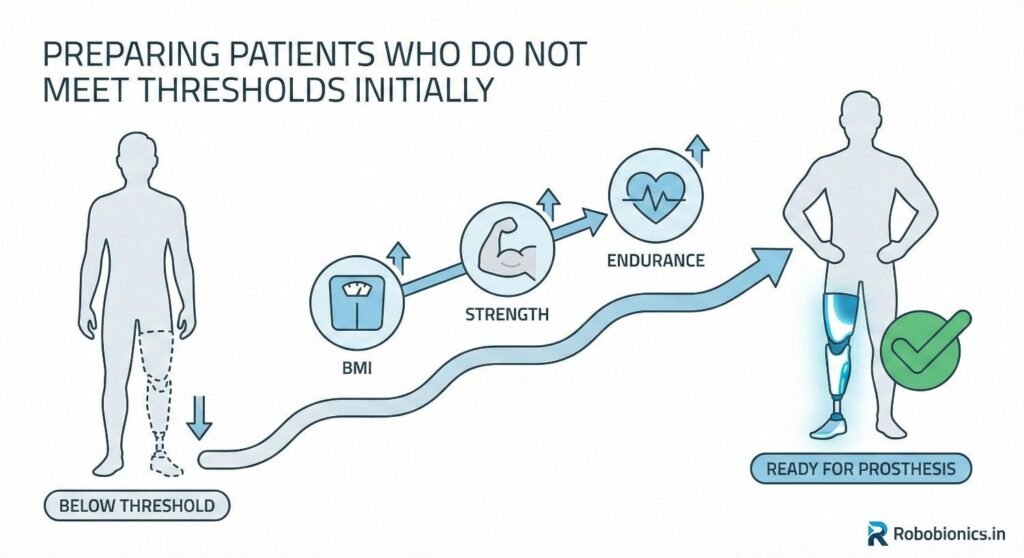
Many patients do not meet BMI, strength, or endurance thresholds at the first assessment, and this should never be framed as failure.
Physical readiness is a process that unfolds over time, especially after illness, injury, or long periods of inactivity.
When doctors present readiness as something that can be built, patients feel encouraged rather than rejected.
This mindset shift is critical for motivation.
Patients are more willing to engage in conditioning when they understand it leads directly to safer prosthetic use.
Clear explanation transforms delay into purposeful preparation.
Targeted conditioning before prosthetic fitting improves outcomes significantly.
Exercises focus on core stability, remaining limb strength, and basic cardiovascular tolerance.
These areas directly support prosthetic control.
Programs should be simple and consistent.
Overly complex routines reduce adherence.
Progress should be gradual and closely monitored.
Doctors should work closely with therapists during this phase.
Regular feedback helps adjust intensity.
Small gains compound over time.
BMI-related challenges often reflect nutritional or medical issues.
Poor nutrition limits muscle gain and endurance.
Addressing this early improves physical readiness.
Medical optimization may include managing anemia, pain, or breathing issues.
These factors quietly reduce capacity.
Treating them improves training response.
Doctors should coordinate with nutritionists and physicians.
Integrated care accelerates readiness.
The body performs better when supported holistically.
Prosthetic weight directly affects endurance and joint stress.
Heavier devices increase energy use during walking and standing.
Patients with limited endurance feel this quickly.
For borderline candidates, lighter designs improve tolerance.
Reduced weight lowers fatigue and improves confidence.
This can be the difference between use and abandonment.
Doctors should consider total system weight, not just components.
Every gram matters for some patients.
Design choices should reflect physical reserve.
Socket design must match body composition and strength.
Low BMI patients need careful pressure spread to avoid pain.
High BMI patients need secure suspension to control movement.
Poor socket match increases effort and discomfort.
This drains endurance and reduces wear time.
Thresholds guide safer socket strategies.
Doctors should expect more adjustments in borderline cases.
Frequent review prevents injury.
Comfort supports consistency.
Components are rated for specific weight and activity levels.
Using components near their limits increases wear and failure risk.
This is especially important in high BMI patients.
Doctors must ensure ratings exceed patient demands.
Safety margins protect both user and device.
Under-rating is a common but avoidable mistake.
Strength and endurance also guide component choice.
Higher demand requires more robust systems.
Matching ratings prevents breakdown.
Early prosthetic training should respect endurance limits.
Long sessions may appear productive but cause delayed fatigue.
This leads to soreness and reduced confidence.
Short, frequent sessions are often safer.
They allow recovery between efforts.
Learning improves when fatigue is controlled.
Doctors should guide therapists on pacing.
Endurance thresholds inform session length.
Structure prevents overload.
Recovery time is a key endurance indicator.
Patients who need excessive rest after training may be overloaded.
This signals need for adjustment.
Doctors should ask about next-day fatigue.
Lingering exhaustion suggests poor tolerance.
Plans should be revised promptly.
Good recovery predicts sustainable use.
It shows the body is adapting.
This is a positive sign.
Daily wear time should increase slowly.
Jumping to full-day use too soon overwhelms the body.
This often leads to setbacks.
Incremental increases allow tissues to adapt.
Muscles and joints need time.
Patience improves durability.
Doctors should set clear milestones.
Patients appreciate structured progression.
This builds trust and confidence.
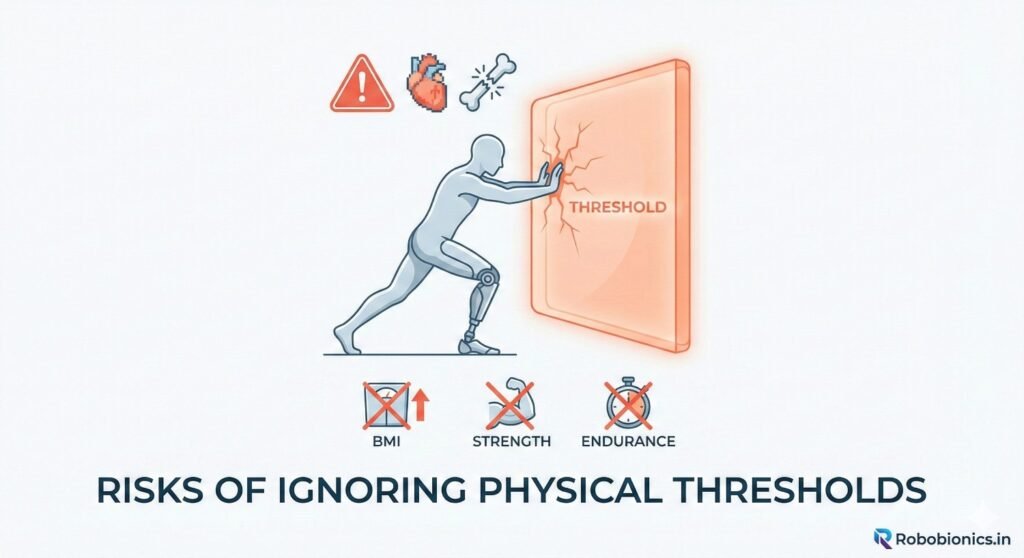
When strength or endurance is inadequate, balance suffers.
Falls become more likely, especially in lower limb users.
Injuries delay recovery significantly.
Falls also damage confidence.
Fear reduces willingness to continue training.
Prevention is far easier than recovery.
Thresholds exist to reduce this risk.
Ignoring them undermines safety.
Doctors must advocate for caution.
Compensating for weakness or poor endurance stresses other joints.
Back pain, knee pain, and shoulder strain are common results.
These issues often appear weeks later.
Chronic pain reduces prosthetic use.
Patients begin avoiding activity.
This leads to deconditioning.
Early threshold-based planning prevents these cycles.
Balanced load protects the body.
Comfort supports consistency.
One of the most common outcomes of ignoring thresholds is abandonment.
Patients stop using the prosthetic because it feels exhausting or painful.
This is often misinterpreted as lack of motivation.
In reality, the body is signaling overload.
Listening to these signals matters.
Threshold-based planning prevents wasted effort.
Abandonment also affects emotional health.
Patients feel they have failed.
Proper planning avoids this harm.
Discussions about BMI, strength, and endurance must be handled carefully.
Patients may feel judged if language is poorly chosen.
Doctors should focus on safety and success.
Explaining thresholds as protective tools helps.
Patients understand that readiness prevents injury.
Respect builds cooperation.
Avoid medical jargon during discussion.
Simple explanations work best.
Clarity reduces anxiety.
Goals should be specific and achievable.
For example, improving standing time or reducing fatigue.
Concrete targets feel manageable.
Shared goals create partnership.
Patients feel involved in decisions.
This increases adherence.
Doctors should celebrate small improvements.
Progress motivates continued effort.
Positive reinforcement matters.
Physical readiness takes time.
Doctors must be honest about this.
Unrealistic timelines lead to frustration.
Explaining why time is needed builds patience.
Patients accept delays when reasons are clear.
Trust strengthens the therapeutic relationship.
Timelines should remain flexible.
Bodies respond differently.
Adaptation improves outcomes.
Older adults often have lower strength and endurance reserves.
BMI may not reflect muscle quality accurately.
Functional testing becomes more important.
Thresholds may be lower, but safety margins higher.
Simple designs and shorter use periods work better.
Goals should reflect daily needs.
Doctors should reassess more frequently.
Capacity can change quickly.
Close monitoring protects safety.
Heart, lung, and metabolic diseases reduce endurance.
These conditions limit prosthetic tolerance.
Thresholds must reflect medical reality.
Collaboration with physicians is essential.
Medical optimization improves readiness.
Ignoring illness increases risk.
Prosthetic goals may need adjustment.
Part-time use may be appropriate.
Quality of life guides decisions.
Bilateral amputees face higher physical demand.
Strength and endurance thresholds must be higher.
Training is more intensive.
Preparation time is often longer.
Patience is essential.
Rushing leads to failure.
Doctors should plan staged fitting.
One step at a time improves success.
Thresholds guide progression.
BMI, strength, and endurance are not fixed.
They change with age, illness, and activity level.
Regular reassessment is necessary.
Weight gain or loss affects socket fit.
Strength changes affect balance.
Endurance shifts affect daily use.
Doctors should schedule periodic reviews.
This prevents surprises.
Proactive adjustment supports longevity.
When capacity declines, goals must adapt.
Reducing wear time or simplifying components may help.
This is not failure but adaptation.
When capacity improves, progression is possible.
Upgrading components may be appropriate.
Flexibility keeps care relevant.
Doctors should normalize these changes.
Patients feel less discouraged.
Adaptation supports long-term use.
Ongoing activity maintains capacity.
Strength and endurance need regular input.
Sedentary habits lead to decline.
Doctors should encourage sustainable activity.
Simple routines work best.
Consistency matters more than intensity.
Education supports independence.
Patients learn to manage their bodies.
This empowers long-term success.
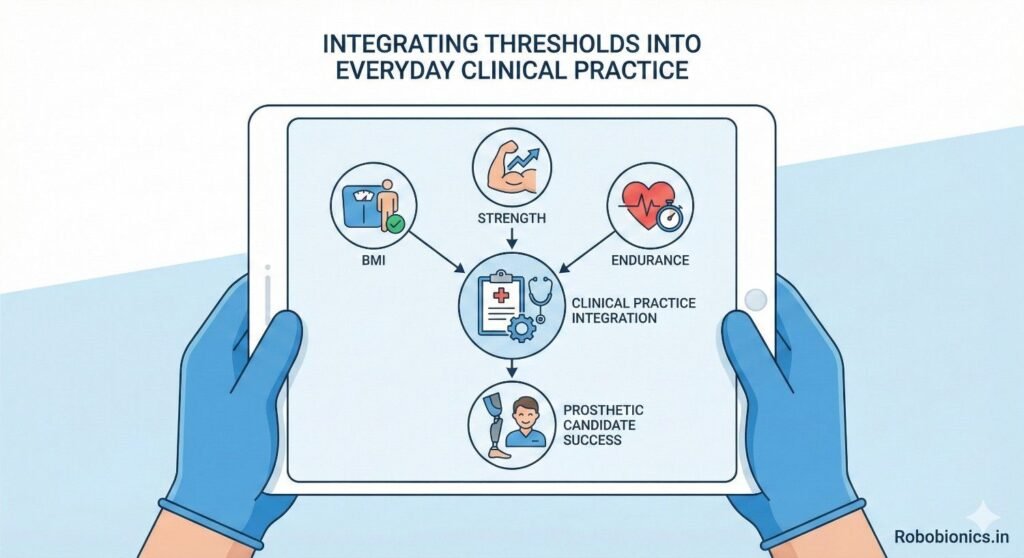
BMI, strength, and endurance should be assessed as routinely as wound healing and limb shape.
When these checks become standard, patients are not singled out or surprised.
Routine assessment normalizes physical readiness as part of safe prosthetic care.
Doctors can use simple tools and observations during regular visits.
This avoids the need for complex testing.
Consistency improves decision quality and documentation.
Embedding thresholds into routine care also improves team alignment.
Therapists, prosthetists, and doctors work from the same baseline.
This reduces mixed messages and confusion.
Threshold-based planning works best when the entire care team shares information.
Strength and endurance findings should inform prosthetic design and training plans.
Clear communication prevents mismatched expectations.
Doctors play a key role in coordinating this process.
By sharing threshold insights early, they guide safer decisions.
Collaboration improves efficiency and outcomes.
Regular case reviews help adjust plans as capacity changes.
This keeps care responsive.
Team alignment protects patient safety.
Clear documentation of BMI, strength, and endurance supports continuity of care.
It allows future providers to understand decision reasoning.
This is especially important in long rehabilitation journeys.
Progress notes should track trends rather than isolated values.
Improvement or decline matters more than single measurements.
Trends guide timely intervention.
Good documentation also supports patient communication.
Patients can see their own progress.
This reinforces motivation and trust.
Physical thresholds should guide, not dictate, decisions.
Rigid cutoffs ignore individual context and potential.
Ethical care requires flexibility.
Doctors must avoid bias based on body size or fitness level.
Every patient deserves individualized assessment.
Thresholds must be applied with judgment.
Context includes age, goals, and support systems.
Numbers alone never tell the full story.
Human insight remains essential.
The purpose of thresholds is safety, not denial.
They help prevent harm and wasted effort.
This must be communicated clearly.
When thresholds are not met, the response should be support.
Preparation and conditioning are the next steps.
Exclusion is rarely the answer.
Patients feel respected when doctors explain this approach.
Trust improves cooperation.
Ethical framing strengthens outcomes.
Ethical care includes reassessment.
What is unsafe today may be safe later.
Capacity can improve with time and effort.
Doctors should plan reassessment points.
This keeps options open.
Hope remains realistic and grounded.
Revisiting decisions also prevents stagnation.
Care evolves with the patient.
Flexibility is a sign of quality care.
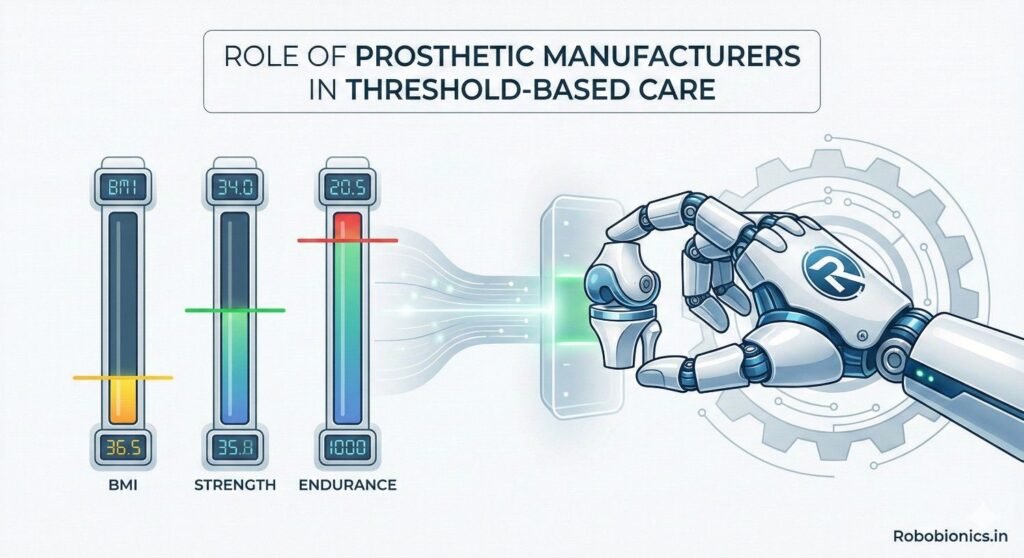
Manufacturers influence how demanding a prosthetic is.
Design choices affect weight, energy cost, and control effort.
These directly impact threshold tolerance.
At Robobionics, we focus on creating designs that respect physical limits.
Lightweight structures and efficient mechanics reduce strain.
Design must serve the body, not challenge it.
Listening to clinical feedback helps refine designs.
Real-world use reveals true demand.
Collaboration improves products.
Manufacturers should provide clear information about component limits.
Weight ratings, activity levels, and intended use must be transparent.
This supports safe prescription.
Clinicians rely on accurate data.
Ambiguity increases risk.
Clear guidance protects patients.
Educational support also matters.
Training clinicians on proper matching improves outcomes.
Knowledge strengthens partnerships.
Prosthetic needs change as physical capacity changes.
Manufacturers must support adjustments and upgrades.
Long-term service matters.
Accessible maintenance reduces downtime.
Reliable support encourages continued use.
Consistency builds trust.
A long-term view aligns with patient journeys.
Care does not end at fitting.
Support must continue.
Physical readiness is the foundation of safe prosthetic use.
BMI, strength, and endurance shape how the body responds to daily demand.
When these factors are assessed honestly, outcomes improve.
At Robobionics, we have seen that respecting physical thresholds prevents injury, frustration, and abandonment.
Patients who are prepared physically adapt faster and use their prosthetics more consistently.
Preparation protects both body and confidence.
Thresholds are not barriers.
They are guides that help patients succeed.
When used with care, clarity, and compassion, they turn prosthetic technology into a true tool for independence rather than a source of strain.

For many clinicians, the surgery is only the first step. What happens after the operation
For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much
Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.