
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
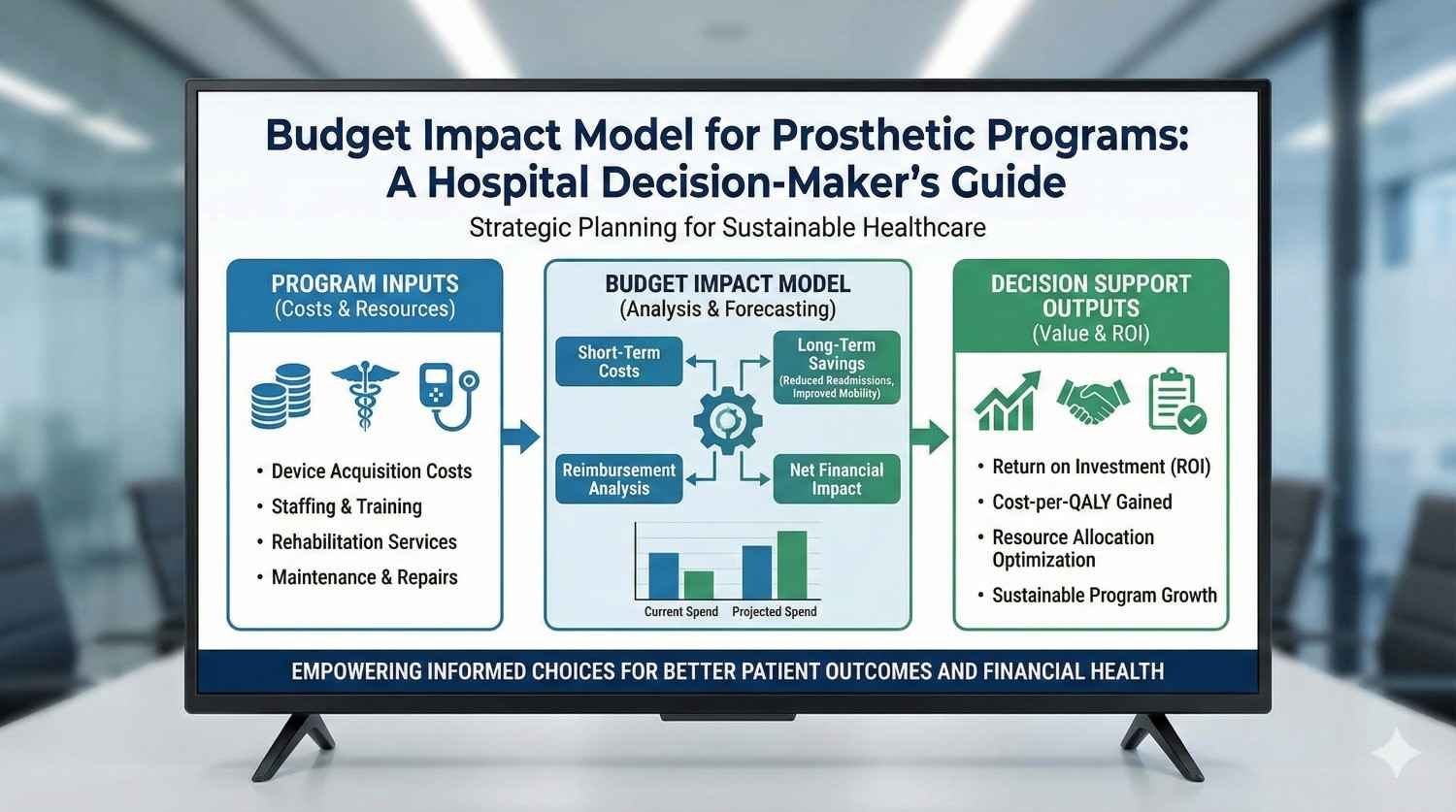
Every hospital that runs a prosthetic program faces the same quiet pressure. Costs are rising, expectations are higher, and decision-makers must justify every rupee spent. At the same time, prosthetic care cannot be treated like a simple purchase. It affects length of stay, readmissions, rehab load, patient satisfaction, and long-term outcomes.
This guide is written for hospital leaders, administrators, and clinical heads who need a clear and practical way to think about budgets for prosthetic programs. We will explain how to build and use a budget impact model in simple terms, grounded in Indian hospital realities. The goal is not theory, but better decisions that balance care quality with financial control.

Prosthetic care in hospitals is no longer about buying a single device for a single patient.
It has evolved into a long-term program that includes surgery, rehab, devices, follow-up, repairs, and outcome tracking.
Without a structured way to see costs over time, expenses appear scattered and hard to control.
A budget impact model brings all these moving parts into one clear view.
Many hospitals still budget prosthetics as a line item under implants or consumables.
This approach hides downstream costs such as longer stays, readmissions, and repeated rehab visits.
When these costs surface later, they feel unexpected and hard to justify.
A budget impact model prevents these surprises by planning ahead.
Hospital leaders today face audits, insurance negotiations, and quality benchmarks.
They are expected to improve outcomes while keeping costs stable or lower.
Prosthetic programs sit at the intersection of clinical care and long-term spend.
Clear financial modeling is no longer optional; it is necessary.
A budget impact model estimates how a prosthetic program will affect hospital spending over time.
It looks at total cost, not just device price.
The model answers a simple question: what happens to our budget if we adopt or expand this program?
This clarity supports confident decision-making.
Cost-effectiveness focuses on value per patient or per outcome.
Budget impact focuses on affordability at the hospital level.
A program can be cost-effective but still unaffordable if cash flow is ignored.
Decision-makers need both views, but for budgeting, impact comes first.
Budget impact models speak the language of finance teams.
They show year-by-year costs and help plan cash flow.
They also allow leaders to test different scenarios safely.
This makes them ideal tools for internal approvals.
The first step is understanding how many prosthetic patients the hospital treats each year.
This includes type of amputation, age groups, and activity levels.
Different patient profiles create very different cost patterns.
Accurate estimates here set the foundation for the entire model.
Hospitals often support multiple prosthetic options.
Basic devices, advanced devices, and specialty components all carry different costs.
A budget impact model should reflect this mix rather than assume a single standard device.
This realism improves forecast accuracy.
Prosthetic programs include surgery, inpatient stay, rehab, and outpatient follow-up.
Each step carries cost and resource use.
Ignoring these elements underestimates the true budget impact.
Hospitals benefit from mapping the full care pathway.
Amputation surgery, wound care, and inpatient monitoring form the initial cost block.
Length of stay varies based on patient stability and rehab readiness.
Prosthetic choices can influence how quickly patients mobilize.
This directly affects inpatient costs.
This includes the prosthetic components, fitting sessions, and initial adjustments.
Costs vary widely depending on technology and customization.
Hospitals should track average costs rather than list prices.
Real-world averages reflect actual spend better.
Rehab is a major cost driver that is often underestimated.
Frequency, duration, and staffing all affect total expense.
Devices that support faster progress can reduce therapy load.
This impact should be captured in the model.
Poor prosthetic outcomes often lead to readmissions.
Falls, skin issues, and pain bring patients back into the system.
Each readmission adds cost and affects hospital metrics.
Budget models should include expected readmission rates.
Unstable patients demand more nursing and therapy supervision.
This increases staff workload and overtime risk.
Stable prosthetic outcomes reduce this burden.
Staff time has real financial value.
Rehab equipment, clinic space, and administrative support all carry overhead costs.
As prosthetic programs grow, these overheads increase.
Ignoring them creates budget gaps later.
Including them supports sustainable planning.
Many budgets are planned one year at a time.
Prosthetic programs, however, create costs and savings over several years.
A one-year view hides long-term trends.
Multi-year models provide better guidance.
Prosthetic components do not last forever.
Hospitals must plan for repairs, replacements, and upgrades.
These cycles affect future budgets.
Planning ahead avoids sudden spikes in spending.
As programs mature, efficiency often improves.
Staff gain experience and pathways become smoother.
Budget impact models should reflect learning curves.
This prevents overestimating long-term costs.

Begin by documenting what the hospital spends today on prosthetic care.
This includes devices, rehab, and complications.
Even rough estimates are useful at this stage.
The goal is to establish a baseline.
Next, clearly define what is changing.
This may be adopting new technology, expanding access, or standardizing care.
Clarity here is essential.
Vague changes produce unreliable models.
The model should compare current practice with the proposed program.
Differences in cost become visible when scenarios are side by side.
This comparison supports clear internal discussions.
Decision-makers respond well to contrasts.
Budget impact models allow safe testing of assumptions.
What if patient volume increases?
What if device mix changes?
These simulations support proactive planning.
Clear models build confidence among leadership teams.
They show that decisions are data-driven, not emotional.
This increases approval speed and trust.
Good models reduce friction.
Budget impact models create a shared language.
Clinicians and finance teams can discuss trade-offs clearly.
This alignment improves program success.
Shared understanding reduces conflict.
Indian hospitals operate in an environment where margins are tight and patient expectations are high.
Unlike systems with universal coverage, many Indian hospitals balance insured, self-paying, and subsidized patients within the same program.
This mix creates unpredictable cash flow, especially for prosthetic care, where costs are front-loaded and recovery extends over months or years.
A budget impact model must reflect this reality rather than assume stable reimbursement.
Patients come from varied economic backgrounds, which directly affects how care unfolds after discharge.
Some patients complete rehab and follow-up as planned, while others stop midway due to cost or travel challenges.
These variations influence readmissions, complications, and overall cost to the hospital.
Models that assume perfect adherence often underestimate true budget impact.
Large urban hospitals may have in-house rehab, prosthetic units, and specialist teams.
Smaller or semi-urban hospitals may rely on visiting prosthetists or external rehab centers.
These structural differences change cost patterns significantly.
A one-size-fits-all budget model does not work across settings.
Many hospitals begin budgeting by negotiating device prices.
While procurement savings matter, they represent only one part of total spend.
Ignoring rehab load, staff time, and complications leads to incomplete planning.
True control comes from looking beyond the purchase order.
Rehabilitation is often treated as a fixed or minor expense.
In reality, therapy duration and intensity vary widely based on device choice and patient confidence.
When rehab demand increases unexpectedly, departments become strained.
Budget models should treat rehab as a variable, not a constant.
Falls, skin issues, and device rejection are not rare events.
Each poor outcome triggers additional care, staff time, and sometimes negative patient feedback.
These costs are real but often hidden.
Including them improves the accuracy of financial projections.
Public hospitals often serve high patient volumes with limited budgets.
Prosthetic programs here focus on access and basic function.
Budget impact models should emphasize scale, standardization, and predictable costs.
Even small efficiency gains can have large system-wide effects.
Private hospitals balance quality, reputation, and financial sustainability.
Advanced prosthetic options may be part of their service offering.
Budget impact models here should capture value from shorter stays and improved patient experience.
Reputation and differentiation also have financial implications.
Trust hospitals often rely on grants, donations, or CSR funding.
Their budgets are sensitive to cost overruns and delays.
Clear modeling helps justify funding requests and manage donor expectations.
Transparency builds long-term support.
Prosthetic technology influences how quickly patients mobilize.
Faster mobility often leads to earlier discharge.
Even one or two days saved per patient adds up over a year.
Budget models should reflect this link clearly.
Unstable prosthetic outcomes increase the likelihood of emergency visits.
Each visit consumes resources and affects patient satisfaction.
Devices that support safer use reduce these downstream events.
This reduction has measurable budget impact.
Patients who struggle with mobility require more supervision.
This increases staff workload and fatigue.
Over time, high strain contributes to burnout and turnover.
While harder to quantify, these effects influence hospital costs.
A one-year budget rarely captures the full impact of prosthetic programs.
Multi-year models allow costs and benefits to balance out.
They also support better planning for replacements and upgrades.
Three to five years is often a practical horizon.
As teams gain experience, efficiency improves.
Rehab protocols become smoother and complications decrease.
Early-year costs may be higher than later years.
Models should reflect this gradual improvement.
Successful programs attract more referrals.
Increased volume can improve efficiency but also stress resources.
Budget impact models should anticipate growth rather than react to it.
Proactive planning avoids bottlenecks.

Decision-makers trust models that show their assumptions clearly.
Hidden assumptions undermine confidence.
Hospitals should document key inputs such as patient volume, device mix, and rehab duration.
Transparency invites constructive discussion.
Budget impact models are not static documents.
They should be updated as data improves.
Regular updates keep decisions aligned with reality.
Living models are more useful than one-time analyses.
Hospitals can use budget impact models to set internal guidelines.
These guidelines support consistent decision-making across departments.
Consistency improves both care quality and cost control.
Policy driven by data is easier to defend.
A budget impact model is only useful if it shapes real decisions, not if it stays on a computer.
Many hospitals build models but fail to integrate them into daily planning, approvals, and reviews.
Implementation means embedding the model into how the hospital thinks about prosthetic care, not treating it as a one-time exercise.
When used correctly, the model becomes a shared reference point rather than a finance-only document.
Hospitals do not need to model every prosthetic scenario at once.
It is often better to start with one segment, such as lower-limb amputees or a specific ward.
This controlled scope allows teams to test assumptions and improve data quality.
Early success builds confidence and momentum for wider adoption.
Budget impact models fail when ownership is unclear.
Hospitals should assign responsibility to a small cross-functional group rather than a single department.
This group typically includes a clinical lead, a finance representative, and a rehab or operations manager.
Shared ownership ensures the model stays relevant and balanced.
Clinicians often worry that financial models will restrict clinical freedom.
Finance teams, on the other hand, worry about uncontrolled spending.
A well-built budget impact model acts as a bridge between these perspectives.
It allows clinical intent and financial reality to be discussed openly.
Models that use only financial terms feel distant to doctors.
Including clinical milestones such as mobility, rehab progress, and complications makes the model relatable.
When clinicians see their world reflected in the numbers, engagement improves.
This shared language strengthens decision-making.
Budget models work best in environments where data is shared without fear.
If complications or delays are hidden, the model becomes inaccurate.
Leadership must emphasize learning rather than punishment.
Honest data improves both care and cost control.
Senior leaders are less interested in technical details and more interested in risk, predictability, and sustainability.
When presenting a budget impact model, focus on how it reduces surprises and supports planning.
Show how different choices affect future budgets, not just current spend.
This framing resonates strongly at leadership level.
Hospitals have broader goals such as patient safety, growth, or community service.
Prosthetic programs should be linked to these goals within the model.
For example, reduced readmissions support both financial health and quality metrics.
Strategic alignment increases leadership buy-in.
Some decisions involve trade-offs, such as limiting certain options or standardizing care.
Budget impact models provide a neutral basis for these discussions.
When choices are backed by data, they feel fairer and more defensible.
This reduces internal conflict.
Hospitals do not operate prosthetic programs alone.
Manufacturers and service partners influence costs, outcomes, and support quality.
Sharing budget impact thinking with partners encourages more transparent discussions.
This often leads to better pricing, service terms, and training support.
Insurers increasingly ask how programs affect overall cost of care.
Budget impact models provide clear answers to these questions.
Hospitals that can demonstrate controlled spend and reduced complications negotiate from a stronger position.
Data-backed discussions build trust.
For trust hospitals and NGOs, donors want to know how funds are used.
A clear budget impact model shows responsibility and foresight.
It explains not just what was spent, but why it was spent that way.
Transparency encourages continued support.
When costs are mapped clearly, patterns emerge.
Hospitals often discover that a small number of issues drive a large share of expense.
These may include extended rehab stays, frequent readmissions, or delayed fittings.
Targeting these pressure points delivers outsized impact.
Variation in care leads to variation in cost.
Budget impact models highlight where outcomes are consistent and where they are not.
Hospitals can use this insight to standardize effective pathways.
Standardization improves predictability and quality.
New technologies or care approaches always carry risk.
Budget impact models allow hospitals to test these innovations in a controlled way.
By modeling best- and worst-case scenarios, leaders can decide where to pilot safely.
This reduces fear of change.
Patient volumes, technology costs, and care practices change over time.
Budget impact models should evolve with these changes.
Regular reviews keep the model aligned with reality.
Stale models lose credibility quickly.
As staff change, knowledge can be lost.
Hospitals should include basic orientation to the budget impact model for new leaders and managers.
This continuity protects long-term planning.
Institutional memory matters.
While models are powerful, they are not perfect.
Unexpected events will still occur.
Leaders should use models as guides, not rigid rules.
Judgment remains essential.

The ultimate goal of a budget impact model is not cost cutting.
It is value stewardship, ensuring that resources deliver the best possible outcomes.
When hospitals think this way, financial discipline and patient care align naturally.
This mindset supports sustainable growth.
Clear models reduce anxiety around spending.
Teams feel more confident making decisions when the financial impact is understood.
This confidence improves speed and quality of action.
Clarity replaces hesitation.
Hospitals known for responsible, transparent programs attract trust.
Patients, partners, and funders prefer institutions that plan thoughtfully.
A strong prosthetic program supported by clear budgeting enhances reputation.
Reputation has long-term value.
Prosthetic programs are complex, long-term commitments, not short-term expenses.
They touch surgery, rehabilitation, finance, staffing, and patient experience all at once.
A well-built budget impact model gives hospital leaders the clarity to manage this complexity with confidence.
It turns uncertainty into structured choice.
At RoboBionics, we work closely with hospitals across India and see how thoughtful budgeting transforms prosthetic care.
When decisions are guided by realistic models, programs become more stable, outcomes improve, and financial stress reduces.
The question is no longer whether hospitals can afford to plan prosthetic programs carefully, but whether they can afford not to.
Every strong budget impact model begins with a clear definition of what the hospital is actually planning to run.
This includes the type of amputations treated, expected patient volumes, technology levels offered, and whether care is inpatient, outpatient, or hybrid.
When scope is vague, budgets drift and accountability weakens.
Clarity at this stage prevents confusion later.
Hospitals should map the entire prosthetic care journey, starting from admission and surgery and ending with long-term follow-up.
This map should include inpatient days, rehab sessions, prosthetic fittings, reviews, and expected complications.
Seeing the full pathway helps leaders understand where costs truly arise.
Partial views always underestimate impact.
Once the pathway is clear, each stage should be assigned a realistic cost based on hospital data.
This includes staff time, bed days, therapy hours, device costs, and overheads.
Perfection is not required; reasonable estimates are enough to guide decisions.
Accuracy improves over time with updates.
Hospitals should always compare current practice with a proposed alternative.
For example, basic prosthetic use versus a more advanced, standardized program.
Side-by-side scenarios make differences visible and easier to discuss.
Decision-making improves when choices are explicit.
No model should assume ideal conditions.
Hospitals should test what happens if volumes rise, follow-up drops, or complications increase.
These stress tests reveal where programs are fragile.
Preparedness reduces future shocks.
Senior leaders rarely have time to review full models.
Hospitals should distill key insights into a one-page summary showing cost trends, risks, and benefits.
Clear visuals and plain language work best.
Good summaries drive faster decisions.
Executives respond strongly to risk reduction.
Budget impact models should show how certain choices reduce unpredictability and downstream expense.
This positions prosthetic programs as risk-managed investments rather than cost centers.
Risk framing builds confidence.
Leaders care about reputation and quality as much as cost.
Connecting budget outcomes to reduced falls, shorter stays, or better recovery strengthens the case.
This reinforces that financial discipline supports patient care.
Alignment matters at the top.
Budgets fail when reviewed only once a year.
Hospitals should revisit prosthetic program data quarterly.
Small adjustments made early prevent large corrections later.
Regular review supports control.
Actual costs will differ from projections.
What matters is understanding why, not assigning fault.
Tracking variance improves future forecasts.
Learning cultures outperform punitive ones.
As teams gain experience, care pathways improve.
Rehab efficiency may rise and complications may fall.
Budget models should reflect these improvements.
Dynamic models stay relevant.

Clear budget models simplify conversations with insurers and auditors.
Hospitals can explain why costs exist and how they are managed.
Transparency reduces friction and delays.
Prepared hospitals negotiate better.
Successful prosthetic programs often grow quickly.
Without planning, growth strains staff and finances.
Budget impact models allow leaders to scale thoughtfully.
Growth becomes intentional, not reactive.
During periods of financial pressure, poorly understood programs are often cut first.
Clear budget models protect prosthetic services by demonstrating value and predictability.
Clarity safeguards continuity of care.
Strong programs survive downturns.
Identify one prosthetic pathway to model first.
Gather rough cost and volume data without waiting for perfection.
Form a small working group with clinical and finance representation.
Start simple and improve gradually.
Document typical patient journeys and common complications.
Share insights about where delays and setbacks occur.
This clinical input strengthens the model immediately.
Collaboration improves accuracy.
Support scenario building rather than exact forecasting.
Help translate clinical steps into financial terms.
Stay open to iteration and refinement.
Partnership beats control.
Prosthetic programs are among the most human services a hospital can offer.
They restore mobility, independence, and dignity, but they also demand long-term planning and responsibility.
A budget impact model does not take compassion out of care; it protects it by making programs sustainable.
When hospitals plan clearly, patients benefit consistently.
At RoboBionics, we work alongside hospitals across India and see the difference thoughtful budgeting makes.
Programs with clear financial vision deliver better outcomes, face fewer crises, and earn deeper trust from patients and partners.
The future of prosthetic care belongs to institutions that combine clinical excellence with financial clarity.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.