
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
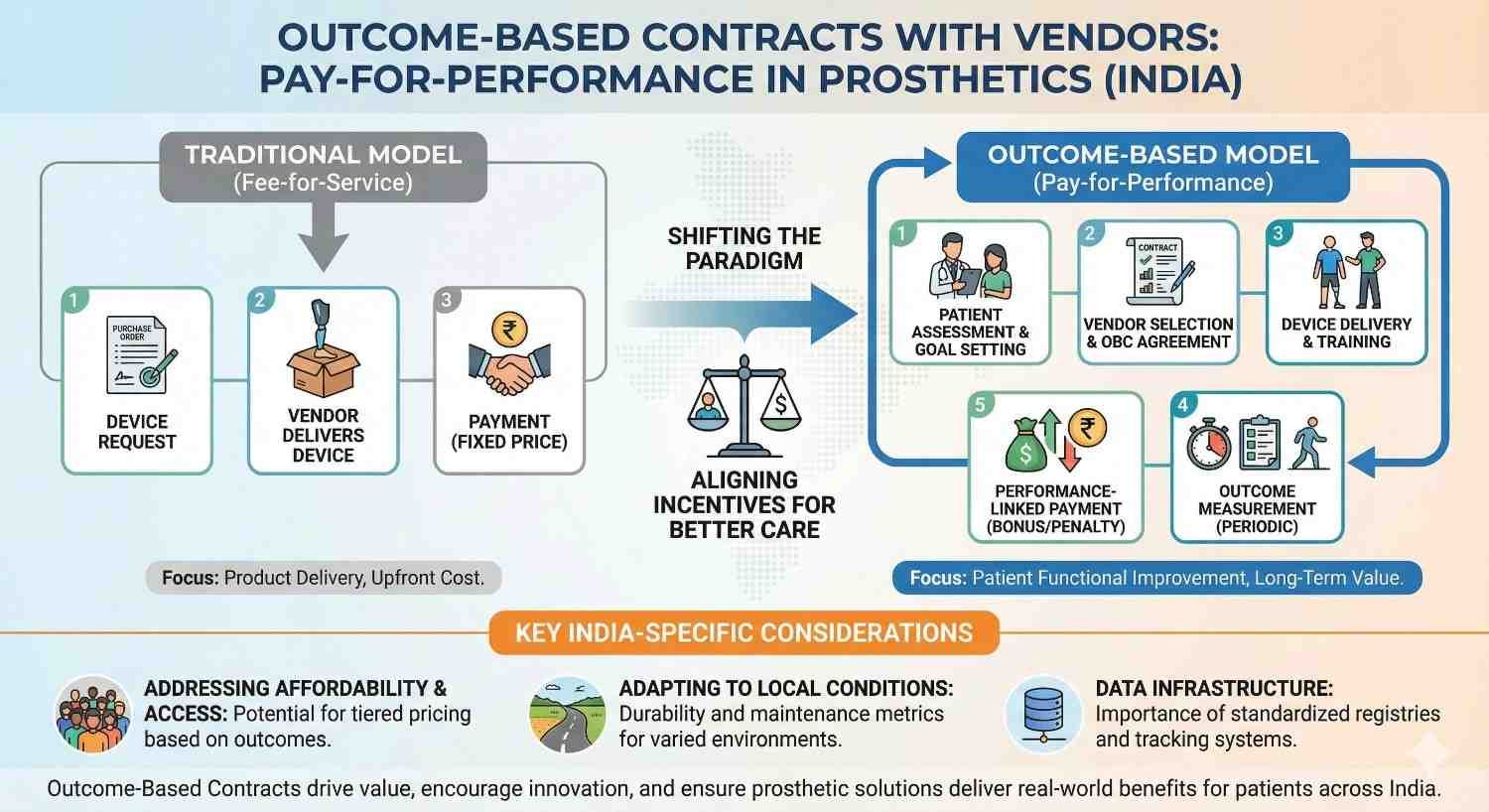
In prosthetic care, everyone wants the same thing: better outcomes for users and fair value for money. Yet most vendor contracts still focus on price and delivery dates, not on how well the prosthesis actually performs in daily life. This gap creates frustration for clinics, payers, and patients alike. Outcome-based contracts offer a better way forward. They link payment to real-world results, not just invoices. This article explains how pay-for-performance can work in Indian prosthetics, using simple ideas, practical steps, and ground realities that clinics and vendors can act on today.

Most prosthetic vendor contracts in India are built around unit price.
The cheapest quote often wins, even when long-term use is uncertain.
This system assumes that delivery equals success.
In reality, a delivered prosthesis that is not used is a failed outcome.
Clinics carry the burden when devices break, fit poorly, or get abandoned.
Vendors are already paid, so incentives stop early.
Once the prosthesis is handed over, follow-up responsibility becomes unclear.
If the user struggles, the clinic absorbs the time and cost.
Vendors may offer support informally, but it is not contractually driven.
This leads to uneven care and strained relationships.
Outcome-based contracts change this balance.
They create shared ownership of success.
A low-cost device that fails early costs more over time.
Extra visits, repairs, and replacements add up quietly.
Traditional contracts do not capture this.
They reward short-term savings over long-term value.
Pay-for-performance forces everyone to look beyond the invoice.
It aligns money with meaningful results.
Outcome-based contracts tie part of the payment to how well the prosthesis performs in real life.
This could include comfort, daily use, durability, or functional gains.
The idea is not to punish vendors.
It is to reward outcomes that matter.
When outcomes improve, everyone wins.
Patients benefit, clinics save time, and vendors build trust.
Many clinics fear outcome-based contracts mean full risk transfer.
That is not necessary or practical.
Most models split payment into parts.
One part is paid on delivery, another after outcomes are met.
This reduces fear and builds confidence.
It allows gradual adoption.
Outcomes must be realistic and measurable.
They should reflect factors within reasonable control.
For example, basic durability or fit stability is fair.
Unrealistic lifestyle expectations are not.
Good contracts choose outcomes carefully.
Fairness keeps partnerships healthy.
Indian prosthetic clinics operate under tight margins.
Costs are rising, but prices are often capped by schemes or competition.
Outcome-based contracts help control hidden costs.
They reduce repeated fixes and rework.
This improves financial stability.
Clinics can focus more on care.
Tele-rehab, digital records, and usage tracking are more common now.
This makes outcome tracking easier.
Even simple follow-up logs provide useful data.
Complex systems are not always needed.
India’s ecosystem is slowly becoming data-ready.
Outcome-based models can now work.
Government schemes and insurers are asking tougher questions.
They want value, not volume.
Outcome-based contracts align well with this shift.
They prepare clinics for future reimbursement models.
Early adopters will have an advantage.
They will already speak the language of outcomes.
A prosthesis that fits well on day one but fails later creates problems.
Fit stability over a few months is a meaningful outcome.
This outcome is influenced by design and materials.
It is reasonable to expect vendor support here.
Tracking comfort complaints and adjustments gives insight.
This data can anchor contracts.
Frequent breakdowns disrupt lives.
They also increase clinic workload.
Contracts can include limits on repair frequency.
Or guarantees on uptime over a period.
This encourages better build quality.
It also improves user confidence.
Usage is a strong signal of success.
If a user stops wearing the prosthesis, something went wrong.
Contracts can define simple check-ins at 3 or 6 months.
Continued use can trigger full payment.
This does not blame the user.
It flags system-level issues early.
User satisfaction is important, but hard to standardize.
Mood, expectations, and life events affect responses.
Using satisfaction alone can create disputes.
It may feel unfair to vendors.
Satisfaction can support other outcomes.
It should not stand alone.
A vendor cannot control patient motivation fully.
Nor can they control unrelated health events.
Contracts should avoid penalizing such situations.
Clear exclusions protect relationships.
Fair contracts recognize shared responsibility.
They do not shift all risk one way.
Outcomes set too far in the future create uncertainty.
They delay closure and payment clarity.
Shorter milestones work better.
They allow learning and adjustment.
Long-term value can still be tracked.
But payments should not wait years.
A common structure works well.
Pay a base amount on delivery.
Hold a second portion for early outcomes.
Release it after fit stability or training completion.
A final portion can link to continued use.
This keeps engagement alive.
Disagreements will happen.
Contracts should plan for them calmly.
Define how outcomes are reviewed.
Specify who decides and how evidence is used.
This reduces tension later.
Clarity upfront saves relationships.
Contracts should be easy to understand.
Complex legal language scares teams.
Simple wording builds trust.
It encourages honest participation.
Outcome-based contracts work best when everyone understands them.
Transparency is essential.
Clinics do not need to overhaul everything.
Start with a pilot.
Choose one vendor and one outcome.
Test the process over a few months.
Learn from this experience.
Refine before scaling.
Most clinics already follow up with users.
This data can support outcome tracking.
No new systems may be needed initially.
Just better use of what exists.
This lowers the barrier to entry.
It makes change feel manageable.
Outcome-based contracts rely on trust.
Start cooperative, not aggressive.
Share data openly.
Discuss issues as partners.
Over time, terms can become clearer and firmer.
Trust grows through action.
Outcome-based contracts often fail when they feel punitive.
If vendors believe the clinic is shifting all risk onto them, cooperation drops and defensive behavior begins.
A shared-risk model works better in prosthetics because outcomes are co-created.
Fit quality, training quality, follow-up discipline, and user education all affect success.
In practice, this means both sides accept partial responsibility.
If outcomes fall short, the response is support and correction first, not immediate financial penalty.
This approach keeps relationships stable.
It encourages problem-solving instead of blame.
Rather than tying payment to a single final outcome, many clinics succeed by linking value to milestones.
Each milestone represents a point where meaningful progress should be visible.
For example, initial fitting success, early comfort stability, and continued usage can each unlock part of the payment.
This spreads risk and keeps engagement active across the care journey.
Milestones also make progress visible.
They turn abstract outcomes into practical checkpoints.
Clinics gain control without micromanaging.
Vendors stay invested beyond delivery.
Refunds create friction and defensiveness.
They feel like punishment even when justified.
Some clinics replace refunds with outcome credits.
If an outcome is missed, the vendor provides extra service, parts, or support instead of cash back.
This keeps value within the care ecosystem.
It directly benefits the patient and clinic workflow.
Outcome credits feel constructive.
They preserve goodwill while enforcing accountability.
Many clinics assume outcome measurement needs new tools.
In reality, most data already exists in routine care.
Follow-up visits, phone calls, and rehab sessions reveal comfort, usage, and issues.
Documenting these consistently creates a usable outcome trail.
The key is discipline, not technology.
Even simple notes build evidence over time.
This approach keeps costs low.
It also fits Indian clinic realities.
Usage does not need sensors to be meaningful.
A short structured conversation can reveal whether a device is being used daily.
Asking about work tasks, travel, and daily routines provides context.
Inconsistencies often signal deeper problems.
Recording this consistently allows trends to emerge.
These trends support fair outcome evaluation.
Clinics should avoid perfection here.
Consistency matters more than precision.
Not every case will be clear.
Some outcomes fall between success and failure.
Contracts should allow for clinical judgement in these moments.
A joint review between clinic and vendor works well.
Honest discussion preserves trust.
Rigid scoring damages relationships.
Outcome-based care thrives on maturity.
Not rigid enforcement.
In India, patients may miss follow-ups due to travel, work, or cost.
This affects outcome measurement.
Contracts should account for this reality.
Penalizing vendors for missed follow-ups is unfair.
Clear clauses that define reasonable follow-up expectations help.
They protect all sides.
Clinics can also use phone-based follow-ups to reduce gaps.
Flexibility improves data quality.
Government schemes and reimbursements cap prices tightly.
This limits how much financial risk vendors can absorb.
Outcome-based contracts must respect these limits.
They should focus more on service quality than deep discounts.
When contracts ignore scheme pressure, vendors disengage.
Balanced design keeps participation healthy.
This realism is essential in India.
Ideal models must bend to context.
A single-room clinic and a multi-city chain cannot use the same contract.
Complexity must match capability.
Smaller clinics should start with very simple outcome terms.
Larger clinics can handle more structured models.
Trying to copy large systems too early causes failure.
Growth should be gradual.
Outcome-based contracting is a journey.
Not a switch.
Outcome-based contracts change how vendors operate.
Sales teams must think beyond delivery.
Support, training, and responsiveness become core value drivers.
This requires internal change.
Vendors who adapt build stronger clinic relationships.
Those who resist lose relevance.
The shift is cultural, not just contractual.
It takes time.
When payment depends on outcomes, vendors must understand their own costs better.
Rework, support calls, and replacements now affect margins directly.
This drives internal efficiency.
It also improves product quality.
Outcome-based models reward disciplined vendors.
They expose weak processes quickly.
This pressure is healthy.
It improves the ecosystem.
Vendors who perform well under outcome-based contracts build reputation.
Clinics trust them more.
This trust leads to repeat business and referrals.
Price becomes less dominant.
Over time, strong vendors gain pricing stability.
Value replaces discounting.
This is how mature markets behave.
India is moving in this direction.

One clinic struggled with frequent post-delivery adjustments.
Staff time was stretched and patients were frustrated.
They introduced a simple outcome clause with one vendor.
Fit stability over eight weeks became a shared goal.
The vendor increased pre-delivery checks and training support.
Adjustments dropped noticeably.
The clinic saved time.
The vendor gained loyalty.
No penalties were applied.
Outcomes improved through alignment.
A multi-city chain faced uneven vendor performance.
Some locations reported frequent repairs.
They introduced milestone-based payments tied to uptime.
Vendors became more responsive.
Poor performers either improved or exited.
Overall quality stabilized.
The chain gained predictability.
Vendors gained clarity.
The system self-corrected.
That is the power of outcomes.
Clinic teams may fear added work or conflict.
Outcome contracts can feel threatening.
Leadership must explain the intent clearly.
The goal is support, not pressure.
When teams see fewer breakdowns and less firefighting, acceptance grows.
Results convert skeptics.
Change must be explained patiently.
People need context.
Too many outcomes create confusion.
Staff stop paying attention.
Clinics should start with one or two clear measures.
Simplicity sustains behavior.
As comfort grows, contracts can evolve.
Rushing causes fatigue.
Outcome-based care is about focus.
Not paperwork.
Contracts should never feel like they are about money alone.
Patient benefit must remain visible.
When staff see better outcomes, motivation increases.
Pride replaces resistance.
Outcome-based models work best when values align.
Care must lead, contracts must follow.
Outcome-based contracts must protect clinics without creating fear for vendors.
The goal is balance, where expectations are clear and enforcement feels fair.
Legal language should support clinical intent, not overpower it.
Short clauses written in plain words often work better than long legal sections.
When vendors understand what is expected, disputes reduce naturally.
Clarity prevents conflict more effectively than threats.
A contract that feels reasonable is more likely to be followed in spirit.
That is where real value comes from.
Prosthetic outcomes depend on many hands.
Contracts should clearly state which parts are vendor responsibility and which remain with the clinic.
For example, device quality and durability may sit with the vendor.
Training adherence and follow-up scheduling may sit with the clinic.
This separation avoids confusion later.
It prevents unfair blame when issues arise.
Clear boundaries support honest review.
They keep partnerships intact during stress.
Indian healthcare faces disruptions like travel barriers, illness, and local shutdowns.
Outcome-based contracts must acknowledge this reality.
Exception clauses protect both sides when events are outside control.
They keep contracts humane and realistic.
Without these clauses, frustration builds quickly.
Flexibility is not weakness, it is wisdom.
Well-written exceptions increase trust.
They show maturity in planning.
Some clinics attempt to push all outcome risk onto vendors.
This almost always backfires.
Vendors respond by increasing prices or reducing support.
Relationships become transactional and tense.
Prosthetic care does not succeed under fear.
Shared accountability produces better results.
Clinics should resist the urge to dominate.
Partnerships outperform power plays.
Clinics sometimes pick outcomes simply because they are simple.
Ease of measurement should not override relevance.
For example, counting visits does not reflect success.
Measuring comfort stability or usage is more meaningful.
Outcome choice shapes behavior.
Poor choices lead to wasted effort.
Clinics must ask whether an outcome truly reflects patient benefit.
That question should guide design.
Nothing damages trust faster than shifting goalposts.
Vendors must know the rules upfront.
If changes are needed, they should apply to future contracts.
Mid-cycle changes create resentment.
Stability encourages investment from vendors.
They plan support based on known terms.
Predictability is a hidden incentive.
It drives better performance.
Many prosthetic clinics compete on price and promises.
Few compete on accountability.
Outcome-based contracts signal seriousness.
They show the clinic stands behind results.
Patients and payers notice this.
Trust grows faster when outcomes are guaranteed in some form.
This differentiation is subtle but powerful.
It builds long-term reputation.
Payers increasingly ask about value.
Outcome-based contracts give clinics a strong answer.
They show that vendors are aligned with outcomes.
This reassures funders.
Clinics that speak this language appear prepared and professional.
They gain leverage in negotiations.
Value-based thinking opens doors.
It prepares clinics for future reimbursement models.
Vendors who succeed under outcome-based contracts become partners.
They invest more in training, support, and innovation.
This loyalty reduces churn.
It stabilizes supply and quality.
Over time, clinics build a trusted vendor ecosystem.
This is hard to replicate.
Strategic relationships beat transactional ones.
They compound value year after year.
Outcome-based contracts work best with shared visibility.
Clinics should share outcome data openly.
This transparency reduces suspicion.
It enables joint problem-solving.
When vendors see patterns early, they can act faster.
This prevents escalation.
Data should be used to improve, not punish.
Tone matters.
One failed case does not define performance.
Trends do.
Contracts should focus on patterns across users.
This reduces emotional reactions.
Trend-based reviews feel fairer.
They encourage systemic improvement.
Clinics should avoid overreacting to outliers.
Perspective is essential.
Outcome tracking must respect patient privacy.
Data should be anonymized where possible.
Contracts should specify data handling clearly.
Trust extends to patients too.
Ethical data use strengthens reputation.
It supports sustainable models.
Care must remain central.
Data is a tool, not a goal.
Staff often think in tasks, not results.
Outcome-based contracts require a shift.
Training should explain why outcomes matter.
Connect daily work to long-term success.
When teams see the link, engagement rises.
Work feels more meaningful.
This shift improves care quality.
It also reduces burnout.
If clinic staff are measured only on volume, outcomes suffer.
Internal incentives should reflect desired behavior.
This does not mean complex systems.
Even recognition and feedback can align effort.
Consistency between external contracts and internal goals matters.
Misalignment creates friction.
Clinics should look inward as well as outward.
Systems must match intent.
Outcome-based contracts take time to mature.
Early results may be uneven.
Clinics should expect learning curves.
Perfection is unrealistic.
Patience allows refinement.
Rushing creates frustration.
Long-term thinking is essential.
Outcome-based care rewards persistence.
At RoboBionics, we believe prosthetic success is shared work.
No device succeeds in isolation.
Our approach to outcome-based partnerships focuses on clarity, fairness, and support.
We align expectations before delivery.
We invest in training, follow-up, and rapid issue resolution because outcomes matter to us.
Our goal is long-term use, not short-term sales.
We work with clinics to define outcomes that are realistic in Indian conditions.
Heat, terrain, and daily work are considered.
When clinics succeed, we succeed.
That belief shapes our contracts and our culture.
Outcome-based contracts are not about shifting risk.
They are about aligning effort.
In prosthetic care, success depends on many small actions over time.
Contracts should reflect this reality.
Clinics that adopt pay-for-performance thoughtfully gain control, credibility, and calmer operations.
They reduce waste and increase trust.
India’s prosthetic ecosystem is evolving.
Value, not volume, will define the next phase.
Outcome-based contracts prepare clinics for that future.
They turn care quality into a shared promise.

Clinics should resist the urge to redesign everything at once.
Outcome-based contracting works best when it begins small and controlled.
Start with one trusted vendor and one outcome that already causes friction, such as repeat adjustments or early repairs.
This keeps the pilot focused and manageable.
The goal at this stage is learning, not perfection.
Early clarity builds confidence for both sides.
Outcomes should be written the way clinicians speak, not the way lawyers write.
For example, instead of abstract quality metrics, describe what success looks like in daily use.
This could mean stable fit without repeated complaints over a defined period.
It could also mean uninterrupted use without breakdowns.
Plain language reduces confusion.
It ensures everyone understands the same goal.
Every outcome needs a review point.
Without timing, outcomes stay vague.
Clinics should align checks with existing follow-ups to avoid extra work.
Three months is often a practical first checkpoint.
Define who reviews the outcome and what evidence is acceptable.
This prevents arguments later.
Structure creates calm.
Ambiguity creates tension.
The financial link does not need to be large.
Even a small portion tied to outcomes changes behavior.
This portion can be released after the outcome is met.
Or converted into service credits if not.
The intent is alignment, not pressure.
Proportion matters more than size.
After the first cycle, clinics and vendors should review results honestly.
What worked and what did not should be discussed openly.
This feedback loop is where real improvement happens.
Contracts evolve through learning, not enforcement.
Refinement builds trust.
Trust sustains the model.
For clinics new to outcome-based contracts, early-stage outcomes work best.
They are closer to delivery and easier to observe.
Examples include fit stability after initial use, reduction in early rework, or completion of training milestones.
These outcomes are influenced strongly by vendor quality and support.
They also build momentum quickly.
Early wins encourage continuation.
Once comfort grows, clinics can include mid-stage outcomes.
These focus on how the prosthesis behaves in daily life.
Examples include device uptime over a few months or continued regular use at a defined checkpoint.
These outcomes reflect real value.
They also encourage vendors to stay engaged beyond delivery.
Support becomes ongoing, not reactive.
In mature relationships, clinics may explore deeper outcomes.
These could include reduced long-term maintenance burden or improved consistency across locations.
Such outcomes require strong data and trust.
They should not be attempted early.
When done well, they create strategic partnerships.
Value compounds over time.
The first conversation sets the tone.
If it sounds like control, resistance follows.
Clinics should frame outcome-based contracts as a way to reduce friction and improve joint success.
The message should be shared benefit, not compliance.
Using examples of past pain points helps.
It grounds the discussion in reality.
Vendors may worry about unfair blame or hidden penalties.
These concerns are valid.
Clinics should listen carefully and adjust design where needed.
Fairness strengthens commitment.
When vendors feel heard, participation improves.
Trust deepens.
Outcome-based contracts must feel mutual.
One-sided designs fail.
Not every partnership will work.
Contracts should allow respectful exit.
Clear exit terms reduce fear of commitment.
They encourage honest experimentation.
Knowing there is a way out makes entry easier.
This is a subtle but powerful enabler.
When outcome alignment improves, clinics notice fewer urgent calls.
Staff spend less time fixing repeat issues.
Schedules become more predictable.
Stress levels drop.
This operational calm is a strong signal of success.
It often appears before financial benefits.
Conversations shift from complaints to improvement.
Vendors become proactive instead of defensive.
Support feels planned rather than reactive.
Trust replaces tension.
This change is noticeable to staff and patients.
Culture improves.
When clinicians trust device performance, they recommend with confidence.
Hesitation reduces.
Patients sense this assurance.
Decision-making becomes smoother.
Outcome-based alignment strengthens clinical authority.
It supports better care.

As more clinics adopt outcome-based thinking, expectations rise.
Low-performing products struggle to survive.
This lifts the overall quality of prosthetic care.
Patients benefit most.
Vendors invest more in reliability and support.
Shortcuts become costly.
The ecosystem matures.
Value replaces noise.
Outcome-based contracts reward solutions that work in real life.
Not just those that look good on paper.
Innovation becomes grounded.
Features must translate to outcomes.
This is especially important in Indian conditions.
Durability and usability matter deeply.
Responsible innovation grows faster under outcome focus.
It serves users better.
Healthcare is moving toward value-based systems globally.
India is no exception.
Clinics that understand outcomes early adapt faster.
They speak the language payers will demand.
Outcome-based vendor contracts are a training ground.
They build skills for the future.
Early movers gain advantage.
Late adopters scramble.
Outcome-based contracts are not a trend.
They are a correction.
They correct the mismatch between payment and performance that has long troubled prosthetic care.
They bring accountability closer to outcomes that matter.
For clinics, they reduce hidden costs, improve predictability, and strengthen credibility.
For vendors, they reward quality, support, and long-term thinking.
For patients, they improve the chances that a prosthesis will truly become part of daily life.
That is the outcome that matters most.
At RoboBionics, we believe prosthetic success should be shared, measured, and supported.
Pay-for-performance is not about pressure, it is about partnership.
When clinics and vendors move together toward outcomes, the entire system becomes stronger, calmer, and more humane.
That is the future of prosthetics in India.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.