Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
Many prosthetic delays do not happen because of surgical problems or device limitations. They happen
When we talk about choosing the right medical device, treatment plan, or rehabilitation path for a patient, we often focus only on the body. We look at age, weight, muscle strength, healing time, and test reports. All of this matters. But there is something equally important that is often missed. That is the patient’s home environment and the people who support them every day.
At Robobionics, after working closely with thousands of patients across India, we have learned one clear lesson. Recovery does not happen only in clinics or hospitals. It happens at home. It happens in daily routines, in small movements, and in the quiet support of family members or caregivers. A patient may have the best prosthetic or medical solution in the world, but if their home setup and support system are not right, the outcome will suffer.
This is why home environment and caregiver support are medically relevant. They directly affect safety, comfort, learning speed, long-term use, and emotional health. They also help doctors, prosthetists, and rehab teams decide what kind of solution is right for a patient. Not every patient needs the same level of technology, training, or follow-up. These decisions should never be made in isolation.
In this article, we will explain why the home setting and caregiver role matter so much in patient selection. We will break this down in very simple words. You will learn what doctors and prosthetic experts look for, how families can prepare, and what practical steps can improve outcomes. This knowledge is useful for patients, families, caregivers, and even healthcare providers.
Patient selection is the process of deciding what medical solution suits a person best. It is not only about whether a device or treatment can work. It is about whether it will work well for that person in their real life. This includes daily habits, family support, living conditions, and emotional readiness.
Many patients meet the medical criteria on paper but struggle later. This usually happens when life outside the clinic is not considered properly. A good selection process reduces risk, improves success, and builds long-term confidence.
The human body does not heal or adapt in isolation. Every movement practiced at home reinforces what was learned in therapy. If the home setup makes movement difficult or unsafe, progress slows down.
Doctors now understand that the best medical decisions look at the full picture. This includes how a patient eats, sleeps, moves, and interacts at home. These factors decide whether recovery becomes smooth or stressful.
Clinics are controlled spaces. Homes are not. At home, floors may be uneven, lighting may be poor, and space may be limited. These differences matter greatly when selecting medical solutions.
Ignoring this gap leads to frustration for patients and families. Understanding it early helps set realistic goals and prevents avoidable problems later.
A safe home is not a luxury. It is a medical need. Slippery floors, narrow walkways, or cluttered rooms increase the risk of falls and injuries. For patients using prosthetics or mobility aids, this risk is even higher.
When doctors evaluate a patient, they must consider whether the home supports safe movement. A device that works well in a clinic may become dangerous in an unsafe home setting.
Many medical solutions need space to use properly. Prosthetic training, exercises, and daily activities all require room to move freely. Small or crowded homes can limit this movement.
This does not mean advanced care is impossible. It means the solution must match the space available. Sometimes simpler or more robust options work better in tight environments.
Good lighting helps patients see and react quickly. Poor lighting increases strain and accidents. Ventilation affects comfort, energy levels, and even wound healing.
These factors are often overlooked, yet they influence how regularly a patient uses their device or follows therapy routines. Comfort encourages consistency, which improves medical outcomes.
The way a patient enters and exits their home matters. Steps, thresholds, and door widths affect independence. If a patient struggles every time they leave the house, motivation drops.
During patient selection, understanding these daily transitions helps decide the level of support and training needed. It also guides home modification advice.
Bathrooms are one of the most dangerous spaces for patients with physical challenges. Wet floors and limited support increase fall risk.
Medical teams often consider whether safety bars, non-slip mats, or seating options are available. If not, recommendations must be adjusted to protect the patient.
The kitchen reflects real-life ability. Can the patient reach shelves, hold utensils, and move safely? These answers guide prosthetic choice and training plans.
A solution that restores kitchen independence often improves mental health and family dynamics. This makes kitchen setup a key evaluation point.
A caregiver may be a family member, friend, or hired helper. They support daily activities, emotional needs, and sometimes medical tasks. Their role is not secondary. It is central.
From a medical view, caregiver presence changes what is possible. It affects how complex or independent a solution can be.
Recovery is not only physical. Fear, self-doubt, and frustration are common. A supportive caregiver helps the patient stay calm and motivated.
Patients with strong emotional support often adapt faster. This is why doctors assess not just physical readiness but emotional backing as well.
Medical success depends on regular practice and proper use. Caregivers help maintain routines. They remind, assist, and encourage.
Without this consistency, even the best technology fails to deliver results. This makes caregiver reliability medically relevant.
Most learning happens at home. Clinics teach basics, but mastery comes from daily repetition. This requires time, patience, and support.
Patients who have help at home learn faster. Those without support may feel overwhelmed and stop trying.
Caregivers often learn alongside patients. They observe training sessions and help repeat them at home. This shared learning improves accuracy and safety.
Medical teams consider whether caregivers can understand and follow instructions. This affects patient selection and training depth.
Mistakes are part of learning. A calm caregiver helps correct errors without fear or pressure. This reduces stress and improves outcomes.
If a patient faces setbacks alone, confidence drops. This emotional risk is taken seriously during evaluation.
Medical solutions vary in cost and maintenance needs. A patient’s financial situation affects long-term sustainability.
Doctors must consider whether families can manage repairs, follow-ups, and replacements. A financially suitable option often leads to better long-term use.
A patient’s role at home and in society matters. Are they working, studying, or managing a household? These roles affect device choice and training needs.
A solution must fit into daily life, not disrupt it. Understanding social roles helps personalize care.
Family beliefs about disability and recovery influence support levels. Encouraging families help patients grow. Doubtful or overprotective families may limit progress.
Medical teams observe these attitudes to predict challenges and plan guidance.

Not every patient has ideal conditions. Recognizing this early prevents unrealistic expectations. It also avoids emotional and financial strain.
Acknowledging limits is not failure. It is responsible medical planning.
Limited support does not mean no solution. It means choosing wisely. Sometimes simpler, durable, and easy-to-use options work best.
Medical relevance lies in matching reality, not chasing complexity.
Support can grow. Training, counseling, and community resources can improve home conditions gradually.
Patient selection can include phased approaches, allowing progress without pressure.
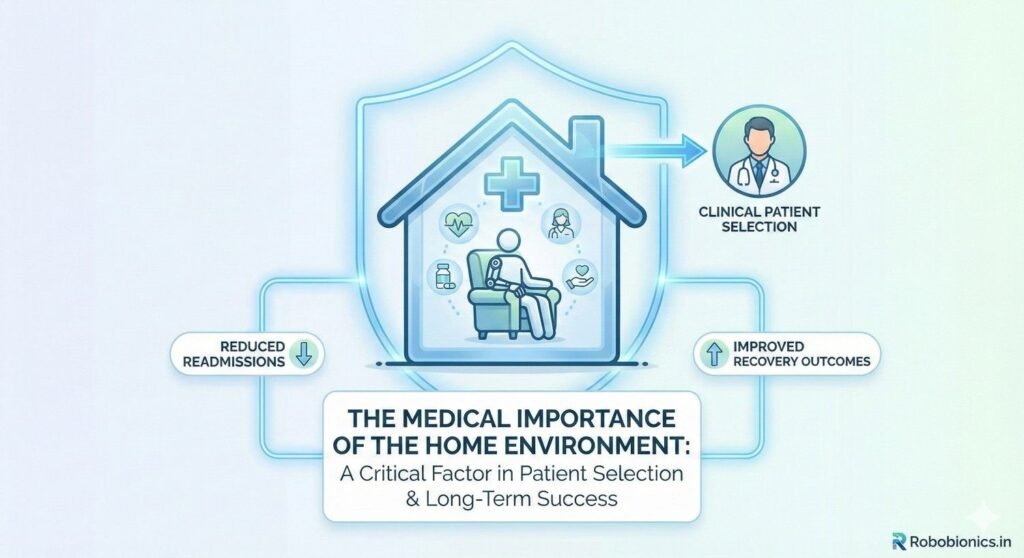
Clinical decisions are meant to protect the patient. They aim to reduce risk and improve quality of life. If home conditions are ignored, even well-planned medical choices can fail.
Doctors and prosthetists do not look only at diagnosis reports. They also think ahead. They imagine the patient waking up, moving through their home, and managing daily tasks. This mental picture guides safer decisions.
Risk is often understood as infection, pain, or device failure. But risk also includes falls, stress, misuse, and abandonment of treatment. These risks rise sharply when home conditions are poor.
A device that demands high precision may increase risk if the patient lives alone or lacks support. Clinical judgment weighs these factors carefully.
Every patient has a different capacity to handle change. Some adapt quickly. Others need time and guidance. Home environment and caregiver support decide how much change a patient can safely manage.
Medical teams aim to match the solution’s complexity with the patient’s real-world capacity. This balance improves safety and success.
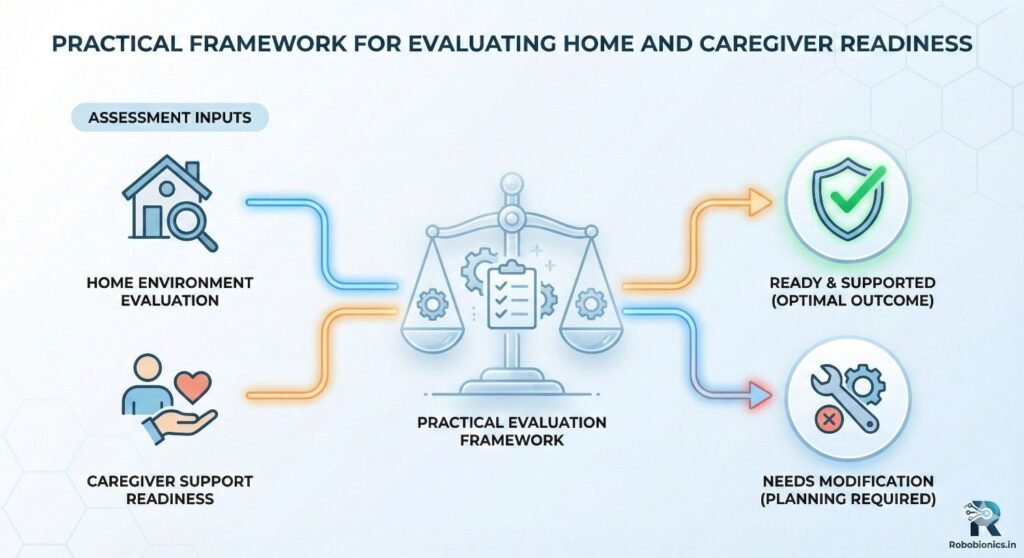
A home evaluation does not always mean a physical visit. It may involve discussions, photos, videos, or detailed questioning. The goal is to understand layout, safety, and daily routines.
Clinicians ask about stairs, bathrooms, lighting, and sleeping arrangements. These details shape the treatment plan.
How a patient moves through their home tells a lot. Do they walk often? Do they sit for long hours? Do they climb stairs daily? These patterns influence device choice.
Medical teams assess whether a solution supports these movements without causing strain or fatigue.
Barriers may be physical, emotional, or social. Narrow spaces, lack of privacy, or family resistance can all block progress.
Identifying these barriers early allows for planning. Sometimes small changes remove big obstacles.
Availability matters as much as willingness. A caregiver may care deeply but have work or health limits. Medical teams consider how much time and energy caregivers can realistically give.
This helps avoid overloading families and setting unfair expectations.
Some caregivers are comfortable with medical tasks. Others feel anxious. Both responses are normal. What matters is honesty.
Clinicians adjust training and support based on caregiver comfort. This improves safety and reduces stress.
Strong emotional bonds help recovery, but over-dependence can slow independence. Medical teams observe these dynamics gently.
The goal is balanced support that encourages growth without pressure.
Advanced technology sounds appealing, but it demands learning, care, and patience. Without proper support, it can overwhelm patients.
Clinicians focus on usefulness, not novelty. The right choice is one the patient will actually use daily.
In homes with limited support, simple and reliable solutions often perform best. They reduce errors and frustration.
Medical relevance lies in long-term use, not short-term excitement.
Patient selection does not have to be final. Many plans allow gradual upgrades as confidence and support grow.
This step-by-step approach respects patient reality while keeping future growth open.
Training plans change based on home help. Patients with strong support can handle faster training. Others need slower, spaced learning.
This flexibility prevents burnout and builds steady confidence.
Skills learned in clinics must be repeated at home. Caregivers often act as gentle reminders and practice partners.
Medical teams design exercises that fit home routines to improve consistency.
Progress is not judged only during visits. Doctors ask about daily comfort, ease, and confidence at home.
This feedback shapes future decisions and adjustments.

Patients need to feel safe to try new movements. Fear of falling or failing stops progress.
A supportive home reduces fear and encourages exploration, which is medically valuable.
Learning new skills is tiring. Frustration is common. Caregivers help patients rest, reset, and continue.
Medical outcomes improve when emotional fatigue is managed early.
Trust grows when patients feel supported. When trust grows, usage increases.
Clinicians value this emotional factor when selecting and recommending solutions.
Sometimes clinical goals are ambitious, but home reality cannot support them yet. Ignoring this leads to failure.
Good medical practice accepts this mismatch and adapts.
Success does not always mean maximum function. Sometimes it means safety, comfort, and dignity.
Clinicians redefine success based on patient reality, not textbook ideals.
A temporary compromise does not mean permanent limits. With time, homes and support systems can improve.
Medical planning often includes future reassessment points.
Prosthetic use is not a one-time medical act. It is a long-term relationship between the user, the device, and their environment. Unlike short treatments, prosthetics become part of daily life.
This makes patient selection more sensitive. A prosthetic must suit not only the body, but also the home, habits, and support system around the user.
Prosthetics are worn for many hours each day. Heat, dust, moisture, and movement patterns affect comfort and durability. Homes with poor ventilation or outdoor work exposure demand tougher solutions.
Medical teams assess where and how the prosthetic will be used. This helps avoid early damage or discomfort.
Some prosthetics are designed for independent users. Others assume some level of help. Choosing the wrong type can create frustration.
If a user lives alone or lacks support, the prosthetic must be easy to manage independently. This decision directly affects long-term success.
True prosthetic learning happens at home. Picking up objects, cooking, dressing, and personal care all take place there.
Training plans are built around these activities. A home that allows safe practice improves learning speed and confidence.
Muscle memory develops through repetition. The home environment decides how often a user practices.
If daily tasks require prosthetic use, learning becomes natural. If the home setup discourages use, progress slows.
Not all homes have large open areas. Training must adapt to available space.
Medical teams design exercises that fit into small rooms without risking safety. This adaptation is key in Indian homes.
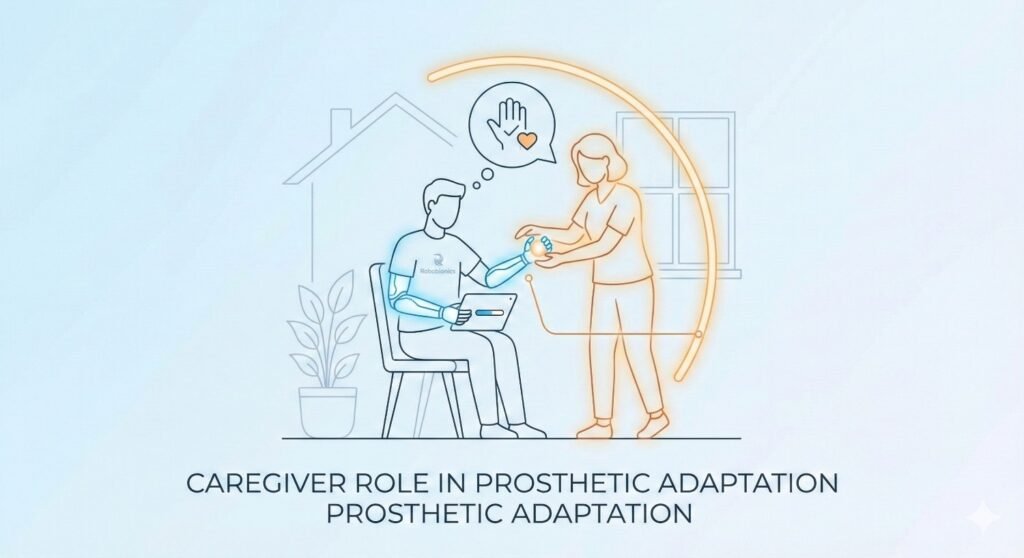
The early phase after fitting is the hardest. The prosthetic feels foreign and tiring. Caregivers provide emotional and physical support during this stage.
Their encouragement often decides whether the user persists or gives up.
Prosthetics need regular cleaning and basic checks. Caregivers often help with these tasks, especially for children or elderly users.
Proper maintenance extends device life and prevents skin issues.
Caregivers notice small changes first. Redness, discomfort, or reduced use are early warning signs.
Reporting these early helps clinicians make timely adjustments.
Many users abandon prosthetics not because of medical failure, but due to daily inconvenience. Heavy devices, difficult controls, or lack of support contribute to this.
Home challenges amplify these issues. Understanding them helps prevent abandonment.
Comfort leads to routine. Routine leads to habit. Habit leads to long-term use.
Homes that support comfortable routines improve adherence naturally.
Acceptance takes time. Supportive families help normalize prosthetic use.
This emotional comfort is as important as physical fit.
Children watch adults closely. Family attitude toward the prosthetic shapes the child’s confidence.
Positive reinforcement at home accelerates adaptation.
Children use prosthetics at school and play, but practice starts at home. Space to play safely matters.
Medical teams consider whether the home encourages active use or restricts movement.
Parents often feel anxious about choosing the right solution. Honest guidance helps them cope.
Clinicians assess parental readiness and provide support accordingly.
Elderly users face balance, vision, and strength challenges. Home safety becomes critical.
Prosthetic selection focuses on stability, simplicity, and comfort.
Many elderly users rely heavily on caregivers. Their availability affects device choice.
Medical teams prioritize ease of use and low maintenance.
Fatigue increases fall risk. Homes must support rest and safe movement.
These factors guide conservative and protective choices.
Many Indian homes are shared by multiple generations. Privacy and space may be limited.
Medical planning respects these realities and avoids unrealistic demands.
Social attitudes influence confidence. Supportive families buffer negative reactions from outside.
This social shield improves long-term use and well-being.
Daily rituals affect routines. Prosthetic use must fit into these patterns.
Clinicians ask about daily schedules to align solutions properly.
Early success is encouraging, but long-term use matters more.
Medical relevance lies in sustained benefit, not quick results.
Regular follow-ups include questions about home experience. This feedback shapes improvements.
Clinicians value honest reports over ideal answers.
Homes, jobs, and families change over time. Prosthetic needs evolve.
Good patient selection allows flexibility for these changes.
A home is not just walls and rooms. It is a living system where habits, emotions, and routines interact every day. Medical teams must see it this way.
Instead of asking whether a home is perfect, the better question is whether it supports safe and regular use of the medical solution.
Asking the right questions often gives clearer answers than long assessments. How does the patient spend their day? Where do they sit, sleep, and work? Who helps them when they struggle?
These questions reveal readiness more honestly than checklists alone.
Every home has strengths. Some have strong emotional support. Others have flexible routines. Some have good space even if resources are limited.
Recognizing these strengths helps build realistic medical plans that respect the patient’s reality.
Families often focus on buying equipment but forget mental preparation. Understanding that adaptation takes time reduces pressure on the patient.
Physically, small changes like clearing walking paths or improving lighting can make a big difference.
Families should know that progress is gradual. Comparing outcomes with others creates stress.
Clear expectations protect emotional health and improve cooperation with medical teams.
Families sometimes hide difficulties out of fear or pride. This harms decision-making.
Honesty allows clinicians to choose safer and more suitable solutions.
Caregivers do not need to be experts. They need to be present, patient, and observant.
Medical teams should explain roles clearly so caregivers feel confident, not overwhelmed.
Helping does not mean doing everything. Allowing patients to try and fail safely builds independence.
Caregivers must learn when to step in and when to step back.
Small discomforts become big problems if ignored. Caregivers should report changes early.
This habit prevents complications and builds trust with clinicians.
Home and caregiver details should be part of medical records. This makes patient selection transparent and ethical.
Formal documentation helps teams stay aligned over time.
Doctors, prosthetists, therapists, and counselors all bring different perspectives.
When they share home-related insights, decisions become stronger and safer.
Recommending a solution that a patient cannot manage is unethical, even if it is advanced.
Ethical care means matching technology to human reality.
At Robobionics, we design with Indian homes in mind. We understand space limits, climate, and daily routines.
This understanding shapes our products and training methods.
Our focus is not just on innovation, but on usability. A solution must feel natural at home.
We prioritize safety, comfort, and gradual learning over complexity.
We see families as partners, not obstacles. Education and empathy guide our approach.
This partnership improves outcomes and long-term satisfaction.
Patient selection is not fixed forever. Life changes, and so do needs.
Regular follow-ups allow adaptation without disruption.
Patients and families should feel safe sharing struggles. Judgment-free communication improves care.
This openness leads to better long-term success.
The goal is always growth. Even small improvements matter.
Long-term planning balances present safety with future independence.
Medical success looks different for every patient. For some, it is full independence. For others, it is comfort and dignity.
Context defines success more accurately than numbers alone.
Pushing beyond limits causes harm. Respecting limits builds trust.
Good medicine respects both ambition and reality.
The best medical solutions fit into life smoothly. They do not demand life to change completely.
This harmony is the true mark of success.
Healing does not stop at the clinic door. It continues at home, every day.
Recognizing this truth improves patient selection and outcomes.
Patients, families, caregivers, and clinicians all share responsibility.
When everyone works together, results improve naturally.
Medical decisions must be careful, informed, and compassionate.
Home environment and caregiver support are not side details. They are central to ethical and effective patient selection.
Many prosthetic delays do not happen because of surgical problems or device limitations. They happen
Traumatic amputations place doctors under intense pressure to save life first, but the decisions made
Amputation after cancer is not just a surgical event. It is the end of one
When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.