
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation

In India, where a person lives often decides how easily they can access a good prosthesis. Big cities offer advanced care but at high cost, while smaller towns struggle with availability despite lower prices. This gap is not just medical, it is economic. The hub-and-spoke model is one of the most practical ways to bridge this divide. This article explains, in very simple terms, how urban and Tier-2/3 cost models differ, why both matter, and how hub-and-spoke economics can expand prosthetic access across India without raising patient burden.
Urban prosthetic centers operate in an environment where fixed costs are high from the very start.
Rent, salaries, utilities, compliance, and marketing all demand steady cash flow.
Because of this, urban centers must maintain high volumes or premium pricing.
Even when patient care is excellent, cost pressure is constant.
These centers often invest heavily in technology and infrastructure.
This improves capability but raises break-even points.
The result is quality with expense.
Access improves, affordability suffers.
Cities attract skilled prosthetists, rehab experts, and technicians.
This concentration allows complex fittings and faster troubleshooting.
However, specialist concentration also increases salary pressure.
Competition for talent pushes costs upward.
Urban centers often bundle advanced diagnostics, gait labs, and rehab under one roof.
This creates convenience but increases overhead.
Patients pay for this ecosystem, whether they need all parts or not.
This drives higher average treatment costs.
Urban patients often expect fast service, minimal waiting, and multiple options.
Meeting these expectations requires larger teams and extended hours.
Service speed itself becomes a cost driver.
More staff and redundancy are needed to avoid delays.
Urban centers also spend more on branding and visibility.
This expense is built into pricing.
The urban model delivers excellence but struggles to scale affordability.
This limits reach beyond city boundaries.

Smaller towns have fewer prosthetic cases per month.
High fixed costs cannot be spread easily.
If an urban-style center is set up in a Tier-2 or Tier-3 city,
it often runs under capacity.
Low utilization leads to financial strain.
Prices rise or services shrink.
This is why many standalone centers fail outside metros.
The economics do not match the environment.
Specialists prefer cities for career growth and lifestyle.
Smaller towns struggle to attract and retain them.
Offering high salaries raises costs beyond what local patients can afford.
Offering lower salaries limits service depth.
This mismatch creates a quality gap.
Patients either travel or compromise.
Urban replication without adaptation increases inequality.
It does not solve access.
Advanced prosthetic services need reliable power, internet, and logistics.
In smaller towns, this infrastructure may be inconsistent.
Urban models assume stability.
When stability fails, service quality drops.
Maintenance and downtime increase costs unexpectedly.
Patients lose trust.
The result is frustration on both sides.
Urban designs break under rural realities.
Rent, wages, and utilities cost less in smaller towns.
This reduces baseline expenses.
However, patient inflow is uneven.
Some months are busy, others quiet.
Revenue volatility is higher.
Cash flow planning becomes critical.
This environment rewards flexible models.
Rigid structures struggle.
While clinic prices may be lower, patient travel costs are often higher.
Many patients travel long distances even within a district.
Lost wages and lodging add hidden expenses.
These costs are rarely counted.
From the patient’s view, total cost may still be high.
Affordability is not just clinic pricing.
Understanding this shifts how access should be designed.
Local presence matters.
In smaller towns, awareness of advanced prosthetics is lower.
Patients often present late.
Late presentation increases complexity and cost.
Rehab becomes harder.
Clinics must invest in education and outreach.
This adds operational effort.
Purely transactional models fail here.
Relationship-based care works better.

The hub-and-spoke model separates what must be centralized from what can be local.
Advanced fabrication, R&D, and specialist review sit at the hub.
Basic assessment, follow-ups, and rehab happen at spokes.
This reduces duplication.
High-cost resources are shared across regions.
Local centers remain lean.
This separation aligns cost with necessity.
It improves sustainability.
When one hub supports many spokes, volumes aggregate.
Procurement, manufacturing, and quality control benefit from scale.
Costs per unit drop without lowering quality.
Savings can be passed on.
Spokes do not need to stock everything.
They draw from the hub as needed.
This reduces working capital pressure.
Cash flows stabilize.
Spokes bring care closer to patients.
Travel reduces, adherence improves.
Patients receive local support while benefiting from central expertise.
This hybrid experience balances quality and cost.
The model avoids building mini-urban centers everywhere.
That mistake is costly.
Instead, it builds a network.
Networks scale better than standalone units.
Urban centers spend heavily on space, staff, and equipment duplication.
Each center carries full capability.
This works only at high volumes.
Outside metros, volumes fall short.
Urban pricing reflects these pressures.
Affordability becomes secondary.
The model is strong but narrow.
It serves those who can reach and pay.
In hub-and-spoke, heavy spending is concentrated.
Spokes remain light and adaptable.
Local centers focus on patient interaction, not capital investment.
This keeps costs down.
Specialist time is used efficiently.
Experts support multiple regions remotely.
Spending follows value creation.
Waste reduces naturally.
When overhead reduces, pricing flexibility increases.
Clinics can offer tiered options.
Patients pay for what they use, not for unused infrastructure.
Transparency improves.
Local presence reduces indirect costs.
Total patient burden drops.
This is the true measure of affordability.
Not sticker price alone.
The hub houses fabrication, advanced fitting expertise, and complex troubleshooting.
It also manages inventory and quality systems.
Training, data analysis, and innovation sit here.
These functions benefit from concentration.
Hubs require strong logistics and digital systems.
They are capital-intensive by design.
However, one strong hub can support many regions.
This justifies the investment.
Hubs attract senior prosthetists and engineers.
Their time is expensive but valuable.
By serving many spokes, their impact multiplies.
This improves cost efficiency.
Workflows should minimize idle time.
Digital scheduling helps.
The hub must feel like a service center, not a bottleneck.
Responsiveness is key.
Logistics define success.
Slow turnaround kills trust.
Hubs must commit to clear timelines.
Predictability matters more than speed.
Spokes should communicate expectations clearly.
Alignment prevents frustration.
When logistics work, the model shines.
When they fail, it collapses.

Spokes should resist feature creep.
They do not need full fabrication or advanced labs.
Their role is assessment, fitting, rehab, and follow-up.
This is where most patient interaction happens.
Keeping spokes simple reduces fixed costs.
It also speeds setup.
Flexibility allows adaptation to local demand.
One size does not fit all.
Local staff understand language, culture, and constraints.
This improves trust.
Training can be standardized and delivered via the hub.
Skill grows over time.
Retention improves when jobs are local.
Costs remain manageable.
Spokes become community anchors.
This strengthens outreach.
Spokes should not stock slow-moving items.
Inventory ties up cash.
Just-in-time supply from the hub works better.
Digital visibility is essential.
Basic consumables can be stocked locally.
High-value items should remain centralized.
This balance protects cash flow.
It reduces waste.
Local spokes reduce long-distance travel.
Patients save money and energy.
Follow-ups become feasible.
Adherence improves.
Lost wages reduce.
Family disruption lowers.
These indirect savings are significant.
They often exceed clinic price differences.
Patients build relationships with local teams.
Trust grows.
The hub supports behind the scenes.
Care feels seamless.
Continuity improves outcomes.
Better outcomes reduce long-term costs.
This virtuous cycle is powerful.
It sustains the model.
When services are structured, patients know what to expect.
Surprises reduce.
Pricing can be staged.
Payments align with progress.
Financial planning becomes possible.
Stress reduces.
Predictability is a form of affordability.
Patients value it deeply.
Poor communication between hub and spokes causes delays.
Blame follows.
Clear protocols are essential.
Roles must be defined.
Digital systems help but culture matters more.
Teams must collaborate.
Without coordination, the model fails.
Structure alone is not enough.
As spokes grow, hub capacity must scale.
Underinvestment creates bottlenecks.
Planning must anticipate growth.
Reactive expansion is costly.
Hubs should monitor load carefully.
Data guides decisions.
Balanced growth keeps service smooth.
Neglect creates friction.
Quality variation across spokes damages trust.
Patients notice inconsistency.
Standard training and audits are necessary.
Feedback loops help.
Quality must feel uniform, even if delivery is local.
This is non-negotiable.
Consistency protects the brand.
It protects patients.
A standalone urban prosthetic center usually carries high fixed monthly expenses that remain constant regardless of patient volume. Rent, senior staff salaries, equipment maintenance, and compliance costs must be paid even during slow months. To remain viable, such centers depend on steady footfall and often price services higher to protect margins. This structure works in dense cities where patient inflow is reliable, but it becomes fragile when replicated in smaller towns with uneven demand.
In contrast, a spoke clinic in a hub-and-spoke system operates with far lower fixed costs because it does not duplicate advanced fabrication or senior specialist presence. Its primary expenses are local staff, basic equipment, and day-to-day operations. When patient volumes fluctuate, the spoke absorbs this variation more easily. The heavy costs sit at the hub, where aggregated demand from many spokes smooths revenue patterns. This difference in cost absorption is the core reason hub-and-spoke models scale more sustainably in Tier-2 and Tier-3 settings.
In an urban standalone model, the cost per patient includes a share of every duplicated capability, whether the patient uses it or not. Advanced tools, idle specialist time, and underused space are silently embedded in pricing. Even when care is efficient, overhead allocation pushes average costs higher. Patients effectively subsidize the infrastructure itself.
In a hub-and-spoke model, cost per patient reflects actual service use more closely. High-value functions such as fabrication, design, and complex troubleshooting are spread across many patients and locations. Spokes charge mainly for interaction, fitting, and follow-up. This separation allows providers to offer advanced prosthetics at lower effective cost without reducing quality. The patient pays for care, not for unused capacity.
Urban centers face constant break-even pressure, which can influence clinical and operational decisions. There is often an unspoken push to maximize utilization of expensive assets, sometimes leading to over-scheduling or limited flexibility for low-paying cases. While most centers maintain ethical standards, the financial tension is real.
Spoke clinics experience less of this pressure because their cost base is lighter. They can afford to be patient, spend more time on counseling, and accommodate lower-income cases without threatening viability. The hub carries the capital burden and can plan for it strategically. This redistribution of pressure changes the care experience in subtle but important ways.

Consider a strong prosthetic hub located in a metropolitan city with good logistics connectivity. This hub invests in skilled prosthetists, advanced manufacturing, and quality systems. Instead of opening full-scale branches in nearby districts, it partners with or sets up small spoke centers staffed by trained local clinicians.
Patients in these districts receive assessment, fitting, and follow-up locally. Only complex steps or fabrication flow through the hub. Turnaround times are predictable because logistics are planned centrally. For patients, the experience feels local and personal, while the technical depth remains high. For the provider, costs remain controlled because expensive capabilities are not duplicated across districts.
In some regions, patient volumes are too low to justify permanent centers. A hub-and-spoke approach allows flexible spokes such as periodic camps or shared clinical spaces. These spokes rely heavily on the hub for planning, fabrication, and specialist oversight.
Although the spoke presence is limited, patients still benefit from structured access to advanced prosthetics. Travel reduces compared to city-only models, and care continuity improves through scheduled follow-ups. This flexibility would be impossible under a standalone urban model, which requires constant volume to survive.
In purely urban models, patients often delay care until they can afford travel, time off work, and city expenses. By the time they arrive, their condition may have worsened. Hub-and-spoke systems reduce this delay by bringing initial access closer to home.
Earlier engagement improves outcomes and reduces long-term cost. Patients feel less intimidated by the process and are more willing to ask questions. This behavioral change is a direct result of economic design, not clinical innovation alone.
A hub must be designed with future spokes in mind, not just current demand. Underestimating growth leads to congestion and delays that undermine the entire network. Providers must invest in scalable workflows, digital coordination, and training pipelines from the beginning.
Capacity planning includes not just physical space, but also specialist time, logistics partnerships, and quality assurance processes. When these elements scale smoothly, the hub can support many regions without losing responsiveness. This foresight separates sustainable networks from those that struggle under success.
Digital tools allow specialists at the hub to support spoke clinics without constant travel. Case reviews, fit assessments, and rehab guidance can be delivered remotely when appropriate. This extends expertise across geography while controlling cost.
Digital support also standardizes decision-making and reduces variation. Spokes feel supported rather than isolated, and patients benefit from consistent quality. The technology itself is not the value; the workflow design is.
Training local clinicians is one of the most powerful roles of the hub. Instead of hiring fully formed specialists in every town, providers invest in structured training and mentorship. Skills grow locally while standards remain centralized.
Over time, this creates a distributed but competent workforce. Costs remain manageable, and retention improves because opportunities exist closer to home. Training is not an expense in this model; it is a multiplier.
When care is local and structured, patients spend less on travel, accommodation, and lost wages. These indirect savings are often larger than differences in clinic pricing. From the patient’s perspective, affordability improves even if the prosthesis itself is advanced.
Patients also avoid emergency travel for repairs or adjustments because support is nearby. This reduces stress and improves adherence. Total cost of ownership becomes predictable and manageable, which matters deeply for long-term acceptance.
Hub-and-spoke systems allow patients in smaller towns to access a range of prosthetic options that would otherwise require city travel. Choice expands without forcing patients into unfamiliar environments or high-risk spending.
This balance empowers patients to select solutions that fit their lives rather than their geography. Economic design becomes a tool for equity. Access improves without compromising safety.
When patients know that follow-up and support are available locally, they are more confident in committing to treatment. Fear of being stranded with a device they cannot maintain reduces significantly.
This confidence leads to earlier decisions and better outcomes. It also reduces the emotional burden on families. The economics of access directly shape trust.
As networks grow, communication can become strained. Delays, unclear responsibilities, or inconsistent information quickly erode trust. Providers must invest in clear protocols and regular coordination.
This includes shared documentation, defined escalation paths, and regular performance reviews. Without these, the model loses its advantage. Structure must be supported by discipline.
While standard processes ensure quality, local adaptation is necessary for cultural and logistical reasons. Over-standardization can feel rigid and alienating to local communities.
Providers must allow spokes some flexibility in patient engagement while maintaining core clinical standards. This balance requires judgment and feedback, not rigid rules.
If the hub becomes too remote or unresponsive, spokes may feel unsupported. Patients may perceive delays as neglect rather than logistics. Maintaining a service mindset at the hub is critical.
Responsiveness, clear communication, and accountability keep the model humane. Economic efficiency should never feel cold or distant.
From a policy point of view, urban-centered prosthetic delivery creates visible imbalance. Services cluster where infrastructure and specialists already exist, while large populations in smaller towns remain underserved. Even when government schemes fund devices, access remains uneven because the delivery system itself is centralized. Policymakers see rising spend without proportional reach, which raises concerns about efficiency and equity.
Urban-only models also inflate scheme costs indirectly. Patients must travel, stay overnight, and often require repeated visits. These indirect costs are not always captured in official budgets, but they affect utilization and satisfaction. When beneficiaries delay or drop out, schemes appear less effective. This is why policymakers increasingly look for delivery models that spread capability geographically without duplicating cost-heavy infrastructure.
Hub-and-spoke models align well with how public health systems already function in India. Many government programs rely on tertiary centers supporting district and block-level facilities. This structure is familiar to administrators and easier to integrate into existing planning frameworks.
In prosthetics, a central hub can meet quality and compliance requirements while spokes embedded in districts handle access and follow-up. This mirrors referral systems used in other specialties. Because the model fits existing governance logic, it faces less resistance during adoption. Familiar structure reduces implementation friction.
Whether public or private, payers prefer predictability. Hub-and-spoke systems offer clearer cost forecasting because high-cost elements are centralized and planned, while variable local costs remain controlled. This makes budgeting easier and reduces unexpected spikes due to underutilized infrastructure.
Payers also benefit from better outcome consistency. When care is closer to patients, follow-up improves and device abandonment reduces. For payers, fewer failures mean fewer repeat claims and complaints. The economics of hub-and-spoke therefore support payer goals even when reimbursement rates remain tight.
India’s policy direction emphasizes local manufacturing and skill development. Hub-and-spoke models support this by concentrating advanced manufacturing and design in hubs while creating employment and skill growth in smaller towns through spokes. This distributed value creation aligns with national priorities.
Instead of importing complete solutions or centralizing all expertise in metros, the model builds domestic capability that scales geographically. Policymakers value this because it strengthens the ecosystem rather than just funding end products. Prosthetics become part of industrial and social development, not isolated healthcare spending.
Many government schemes face a difficult balance between expanding coverage and controlling per-patient cost. Hub-and-spoke systems help resolve this tension. By reducing duplication and indirect patient expenses, overall value improves even if device reimbursement remains unchanged.
For schemes, this means better utilization of allocated funds. More beneficiaries complete treatment successfully, which improves program metrics. Access expands horizontally across districts rather than vertically through higher spending per patient. This is an attractive outcome for administrators under budget pressure.
Central hubs make it easier to collect standardized data across regions. Utilization, outcomes, and service timelines can be tracked consistently. This transparency supports audits and program evaluation, which are critical for public funding.
Spokes feed real-world data into the hub, creating a clearer picture of national or state-level performance. Policymakers increasingly demand this visibility. Hub-and-spoke models provide it without excessive administrative burden at the local level.
In traditional growth models, providers expand by opening full-service centers in new cities. This approach is capital intensive and risky outside major metros. Hub-and-spoke shifts the growth mindset from owning locations to building networks.
Providers invest in process strength, logistics, training, and coordination rather than bricks and mortar everywhere. Growth becomes about reach and reliability, not just physical presence. This change improves resilience and reduces exposure to local market volatility.
Because hubs require upfront investment, providers adopting this model are forced to think long term. Returns come through scale and consistency rather than quick margins. This naturally aligns incentives toward quality, training, and patient retention.
Short-term cost cutting becomes less attractive because it harms the entire network. Providers focus instead on reducing waste, improving turnaround times, and strengthening relationships with spokes. Over time, this creates sustainable advantage that standalone centers struggle to match.
Hub-and-spoke systems allow providers to offer different service levels without fragmenting infrastructure. Basic care can be delivered locally at lower cost, while advanced options remain accessible through the hub. This tiering reflects patient diversity without creating parallel systems.
From an economic perspective, this flexibility is powerful. Providers can serve a wider range of patients without diluting quality or inflating costs. Choice increases, but complexity remains manageable because the backbone is shared.
For clinicians, hub-and-spoke models change how expertise is applied. Instead of being tied to one location, senior clinicians support multiple spokes through structured reviews and scheduled visits. Their time is used where it adds the most value.
Local clinicians handle routine care with clear escalation pathways. This reduces professional isolation and improves confidence. Doctors in smaller towns feel supported rather than stretched beyond scope. The economic model directly supports safer clinical practice.
In standalone centers, clinicians often carry full responsibility for outcomes, operations, and patient expectations. This load is heavy and contributes to burnout, especially in low-volume settings. Hub-and-spoke distributes responsibility across the network.
Support systems, peer review, and centralized troubleshooting reduce individual stress. Clinicians can focus more on patient interaction and less on operational firefighting. This improves job satisfaction and retention, which are hidden but critical economic benefits.
When protocols, training, and oversight are centralized, variation reduces. Patients receive similar standards of care regardless of location. For doctors, this consistency simplifies decision-making and documentation.
Consistency also protects clinicians legally and ethically. When practice aligns with network standards, individual exposure reduces. Economic design thus reinforces professional safety and confidence.

Hub-and-spoke models require significant upfront investment at the hub. Facilities, systems, and senior talent must be in place before spokes generate sufficient volume. This barrier can deter smaller providers or those seeking quick returns.
However, this investment is also a filter. Providers who commit are more likely to build durable systems rather than fragile expansions. Policymakers and partners should recognize this and support credible hubs rather than encouraging thinly spread infrastructure.
In early stages, turnaround times and coordination may be uneven as systems settle. Patients and local partners may compare initial experience unfavorably with established urban centers. Clear communication during rollout is essential to maintain trust.
Providers must resist the temptation to overpromise. Honest timelines and gradual improvement build credibility. Economic sustainability depends on managing expectations as much as managing costs.
As networks expand, there is a risk of losing focus on access and affordability and drifting toward premium positioning. This often happens when hubs chase higher margins or spokes push upgrades aggressively.
Strong governance and values are required to prevent this drift. Economic models must be supported by clear mission alignment. Access should remain a core metric, not just revenue.
In a country as diverse as India, geography has long dictated access to advanced healthcare. Prosthetics should not follow this pattern. Mobility, dignity, and independence are not urban privileges. Economic design plays a decisive role in changing this reality.
Hub-and-spoke models offer a practical way to balance quality and affordability across regions. They recognize that not every function needs to be everywhere, but every patient needs access. This clarity is what makes the model powerful.
No single stakeholder can solve access alone. Providers must design smart networks, doctors must engage confidently within them, and systems must support scale through policy and reimbursement. When these pieces align, access expands naturally.
Economic models are not abstract frameworks. They shape daily patient experiences. Choosing the right model is a clinical decision as much as a financial one.
At RoboBionics, we have built our approach around hub-and-spoke thinking because India demands it. Advanced design, manufacturing, and quality control sit at strong hubs, while local partners and centers bring care closer to patients.
This structure allows us to offer advanced prosthetics at prices that make sense beyond metros, without compromising safety or support. Our focus remains on predictable outcomes, local engagement, and long-term sustainability.
Expanding prosthetic access in India is not about copying urban models everywhere. It is about respecting local realities while sharing national capability. Hub-and-spoke economics make this possible.
When cost structures align with geography, access follows naturally. Patients travel less, adhere more, and trust the system. That is how mobility becomes a right rather than a privilege.

For many clinicians, the surgery is only the first step. What happens after the operation
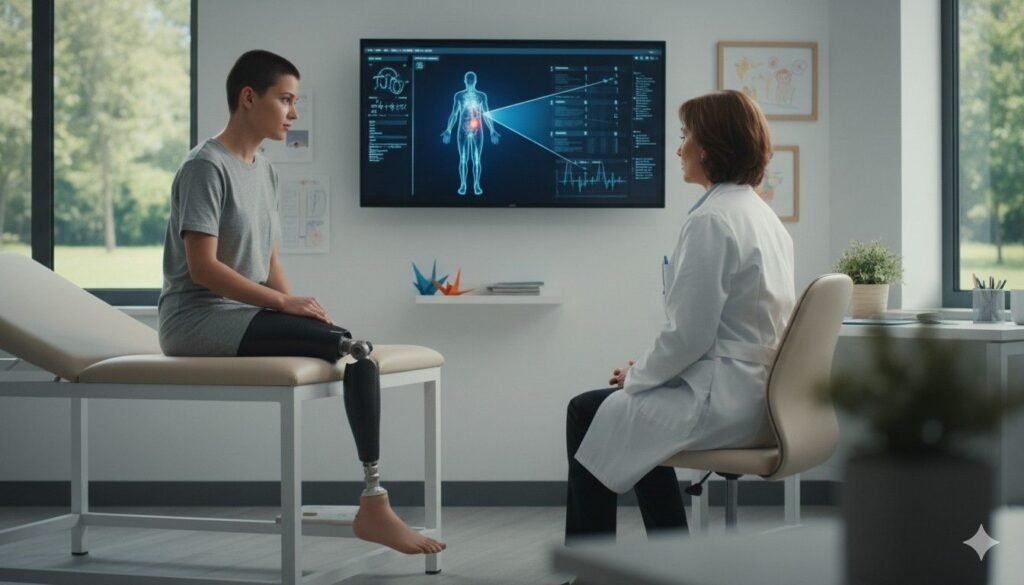
For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much
Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.